Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The risk of cardiovascular disease (CVD), including myocardial infarction and stroke, is higher in SLE than in the general population. The excess risk of premature CVD has been attributed to SLE-related systemic inflammation and its treatment. CVD risk prediction algorithms perform poorly in SLE populations because they do not capture SLE-related inflammation. The purpose of this study was to quantify the excess CVD risk, beyond that predicted by a traditional risk calculator, in strata of patients defined as mild/remission, moderate or severe SLE by the Physical Global Assessment (PGA) of disease activity.
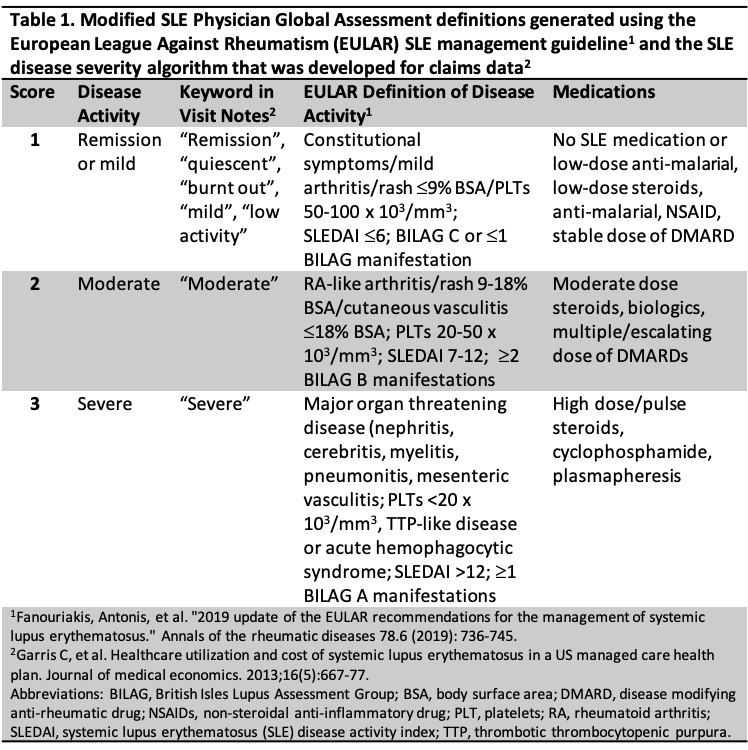
Methods: We included SLE patients enrolled in a local SLE cohort and collected their one-year baseline data on traditional CVD risk factors, demographic and clinical features from the electronic medical record (EMR) at cohort enrollment. Subjects were required to have one or more visits for SLE during the baseline period. Their overall disease activity representing all encounters during the entire baseline year was rated independently by two reviewers (KC and MC) using a modified PGA tool (Table 1). PGA scores ranged from 1 (remission/mild), 2 (moderate), to 3 (severe). A 10-year follow-up period for CVD events began day +1 at end of baseline period (index date). The first MI or stroke in the follow-up period was identified in the EMR using ICD-9/10 codes and adjudicated by medical record review. We excluded subjects with CVD events prior to the index date. Relative excess risk of CVD event in 10 years was determined by comparing the risk expected according to the 2013 American College of Cardiology (ACC) and the American Heart Association (AHA) risk equation and to the observed outcomes, stratified by PGA. The Greenwood-Nam-D’Agostino calibration test was used to compare observed to expected in each PGA category.
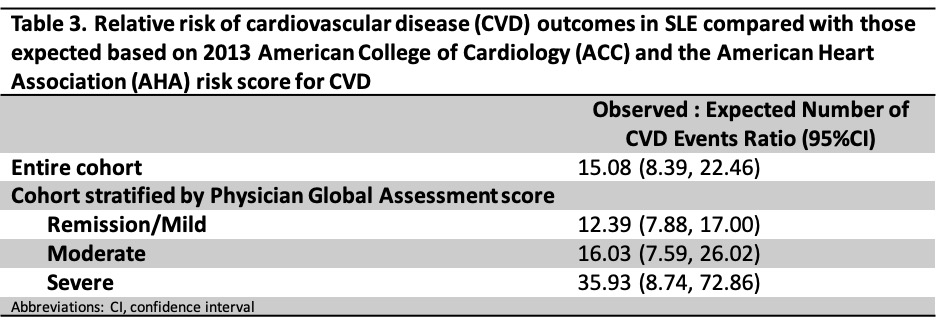
Results: We included 1243 patients; 93.0% female and mean age of 41.6 (SD 13.3) years (Table 2). 80.6% patients had remission/mild disease, while 8.9% had moderate and 10.3% had severe disease. Inter-rater agreement of PGA’s was substantial with 93.5% agreement corresponding to weighted k of 0.75 (SE 0.08, p< 0.001), respectively. There were 212 CVD events, 173 MIs and 64 strokes, over the follow-up period of 8242.92 person-years (PY). The incidence rate (IR) for the entire cohort was 26 [22, 29]/1000 patient PY. When stratified by PGA, the IRs were 24 [21, 28] for remission/mild, 32 [22, 49] for moderate, and 35 [24, 51] for severe. The observed vs expected ratio of CVD events using the ACC/AHA risk equation was highest among patients with severe disease (35.93 [95%CI 8.74,72.86]), followed by moderate (16.03 [95%CI 7.59, 26.02]) and remission/mild disease (12.39 [95%CI 7.88,17.00]) (Table 3). All calibrations were p< 0.01 meaning the calibration of observed events to risk predicted by the ACC/AHA algorithm was significantly off for all PGA categories.
Conclusion: The excess risk of CVD events in SLE patients is underestimated by traditional cardiovascular prediction tools, although the degree of underestimation may be increased in patients with more severe SLE disease activity over the past year. Therefore, more SLE-specific CVD risk prediction algorithms are needed.
To cite this abstract in AMA style:
Choi M, Stevens E, Guan H, Li D, Ellrodt J, Kargere B, Cai T, Yoshida K, Everett B, Costenbader K. Personalizing Cardiovascular Risk Prediction for Patients with Systemic Lupus Erythematosus by Physician Global Assessment of Disease Activity [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/personalizing-cardiovascular-risk-prediction-for-patients-with-systemic-lupus-erythematosus-by-physician-global-assessment-of-disease-activity/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/personalizing-cardiovascular-risk-prediction-for-patients-with-systemic-lupus-erythematosus-by-physician-global-assessment-of-disease-activity/