Session Information
Date: Monday, November 11, 2019
Title: Pediatric Rheumatology – ePoster II: SLE, Juvenile Dermatomyositis, & Scleroderma
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Avascular necrosis (AVN) is a serious comorbidity of juvenile systemic lupus erythematosus (jSLE) associated with disability, impaired quality of life, and increased cost of care. Many factors have been been reported to be associated with AVN risk, with most studies focused on adult SLE. A recent meta-analysis found high maximum and cumulative glucocorticoids (GC) dosage, lupus nephritis (LN), central nervous system disorder, and Cushingoid body habitus to be associated with AVN (Nevskaya et al 2017; Clin Exp Rheumatol; 35:700). The aims of this study were to identify factors associated with AVN risk in jSLE.
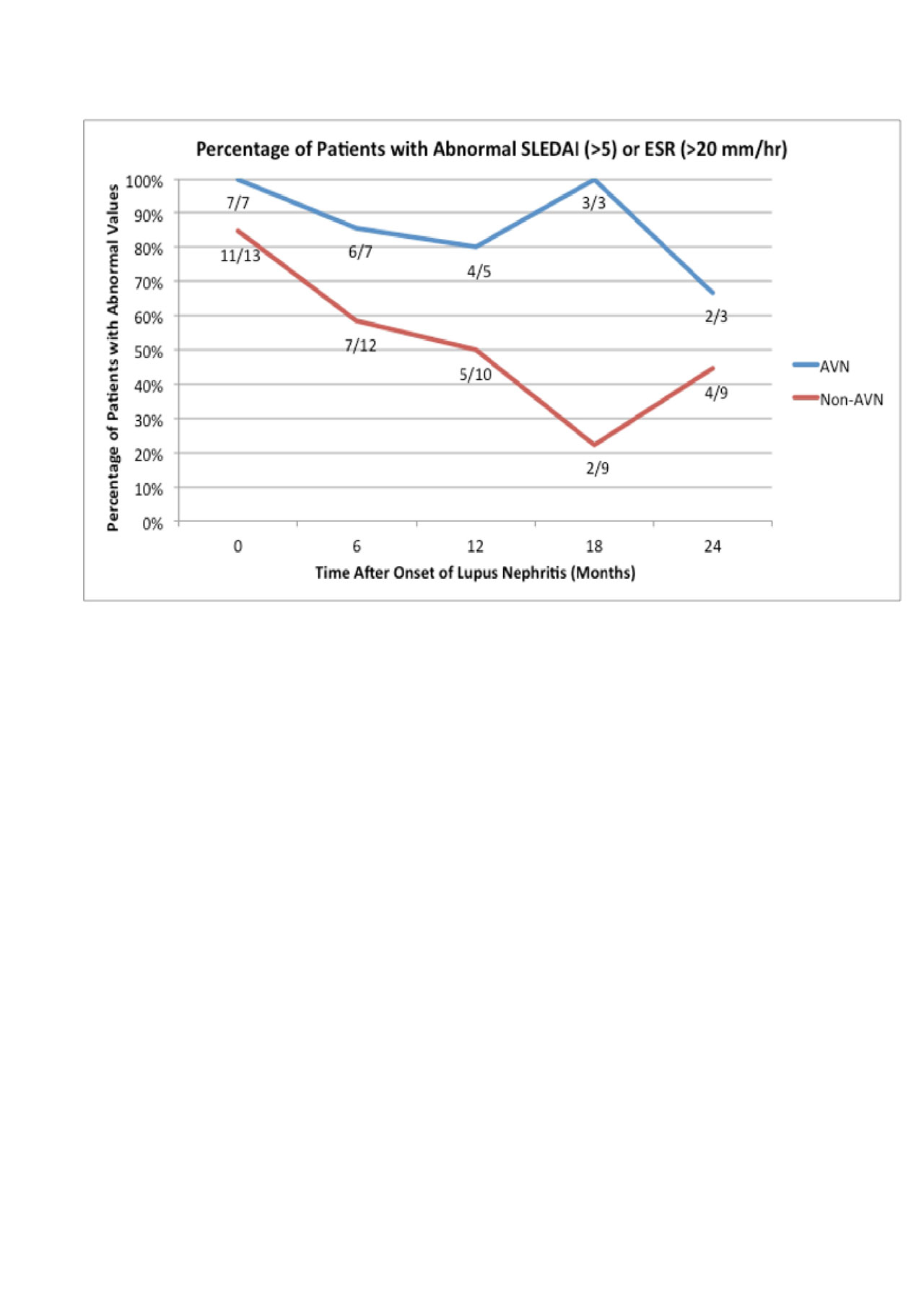
Methods: We conducted a single center retrospective cohort study of jSLE patients seen between 2009-2010. Eligible patients had to fulfill 1997 American College of Rheumatology (ACR) classification criteria for SLE and/or have LN, and been treated with GC. Data was collected from disease onset to AVN development for AVN patients, and to 12/31/10 for non-AVN patients. Onset of LN was considered to be time of renal biopsy. For the subanalysis, the minimum age of disease onset for the comparator group was the youngest age of onset in the AVN group (11 years old). We calculated Systemic Lupus Erythematosus Disease Activity Index (SLEDAI) scores for each 6-month timepoint following renal biopsy based upon reported clinical features and laboratory values within 2 months of timepoint. Active disease was considered to be SLEDAI score >5 and/or erythrocyte sedimentation rate (ESR) score >20. Univariate statistics, two-tailed Fisher’s exact tests, and independent samples t-tests were performed. P values < 0.05 were considered to be significant. Results: Of the 101 jSLE patients identified, 49 fulfilled study criteria, 7 (14.0%) of whom developed AVN. AVN patients had an older age of SLE onset, higher prevalence of LN class III, higher prevalence of neurologic or CNS disorder, and higher mean daily oral GC dose than non-AVN patients (Table). No significant differences were found for gender, race, ethnicity, mucocutaneous involvement, cytopenia, autoantibody pattern, Cushingoid habitus, cumulative GC dose, methylprednisolone pulse treatment, or other treatment (Table). To evaluate for additional factors associated with AVN risk, we did a sub-analysis of patients that had adolescent age of SLE onset and LN (adolescent LN)(Figure). Patients were censored after developing AVN (AVN patients), or at the end of the study period (non-AVN patients). Compared to adolescent LN who did not develop AVN, the AVN group were more likely to have persistently elevated SLEDAI scores and/or ESR values for up to 2 years following onset of LN.
Conclusion: We found older age of SLE onset, LN class III, neurologic/CNS disorder, and higher mean daily GC dose were associated with AVN risk. Patients with AVN were more likely to have persistently active disease following onset of LN than LN patients who did not develop AVN. This suggests that higher disease activity at certain times may also contribute to AVN risk in jSLE. Prospective studies are needed to assess these potential risk factors for AVN development and improve our ability to identify and manage at-risk patients.
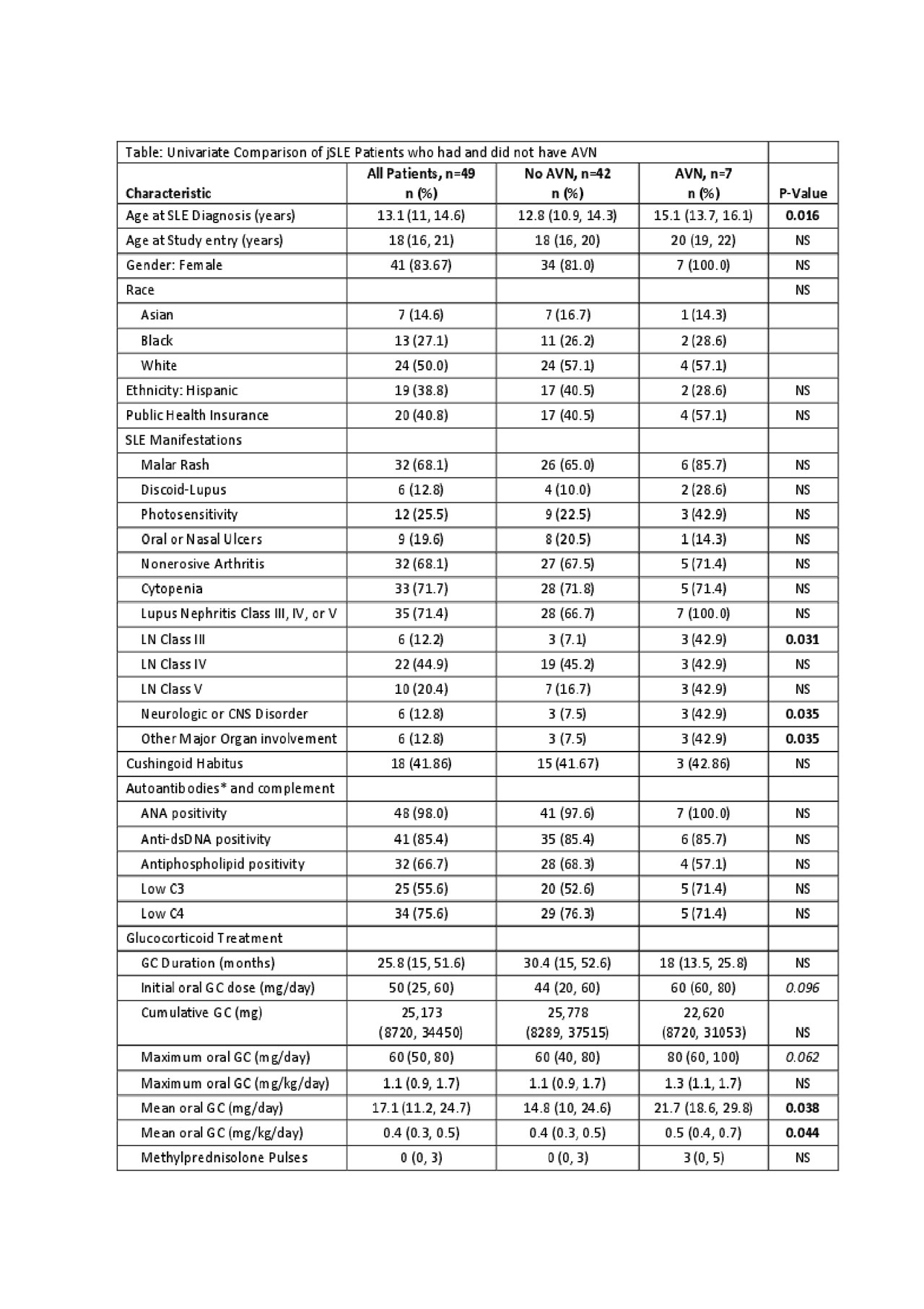
Table 1.final.revised.2019.6.4
To cite this abstract in AMA style:
Hoang A, Yang H, Andrews T, Weiss J, Haines K, Kimura Y, Li S. Persistent Disease Activity Is Associated with Avascular Necrosis Development in Juvenile Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/persistent-disease-activity-is-associated-with-avascular-necrosis-development-in-juvenile-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/persistent-disease-activity-is-associated-with-avascular-necrosis-development-in-juvenile-systemic-lupus-erythematosus/