Session Information
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Perioperative management of anti-rheumatic drugs in rheumatoid arthritis (RA) patients undergoing surgery remains controversial. Previous studies produced conflicting results, and data on non-orthopedic surgeries in RA patients are limited. The objective of the current study was to measure the impact of perioperative anti-rheumatic medication management on the 30-day odds of infection among RA patients undergoing surgery.
Methods: We conducted a retrospective cohort study of seropositive RA patients who underwent musculoskeletal or major organ surgery within the Fairview Health System in Minnesota between January 1, 2010 and December 31, 2017. Each surgical event was identified through the electronic medical record and manually reviewed by two trained clinicians for demographic variables, perioperative medication management, and outcomes. Surgeries were classified into three groups according to anti-rheumatic medication use during surgery: 1. neither DMARD nor biologic (either not prescribed or held for a pre-specified period of time, based on each medication’s dosing schedule and mode of action); 2. DMARD with no biologic; 3. biologic with or without DMARD. The perioperative use of corticosteroids and antibiotics was also recorded. The primary outcome, post-operative infection, included surgical site infections, urinary tract infections, pneumonia, and blood stream infections occurring within 30 days of surgery as defined by CDC criteria. ANOVA, Chi-square tests and logistic regression were used for analyses.
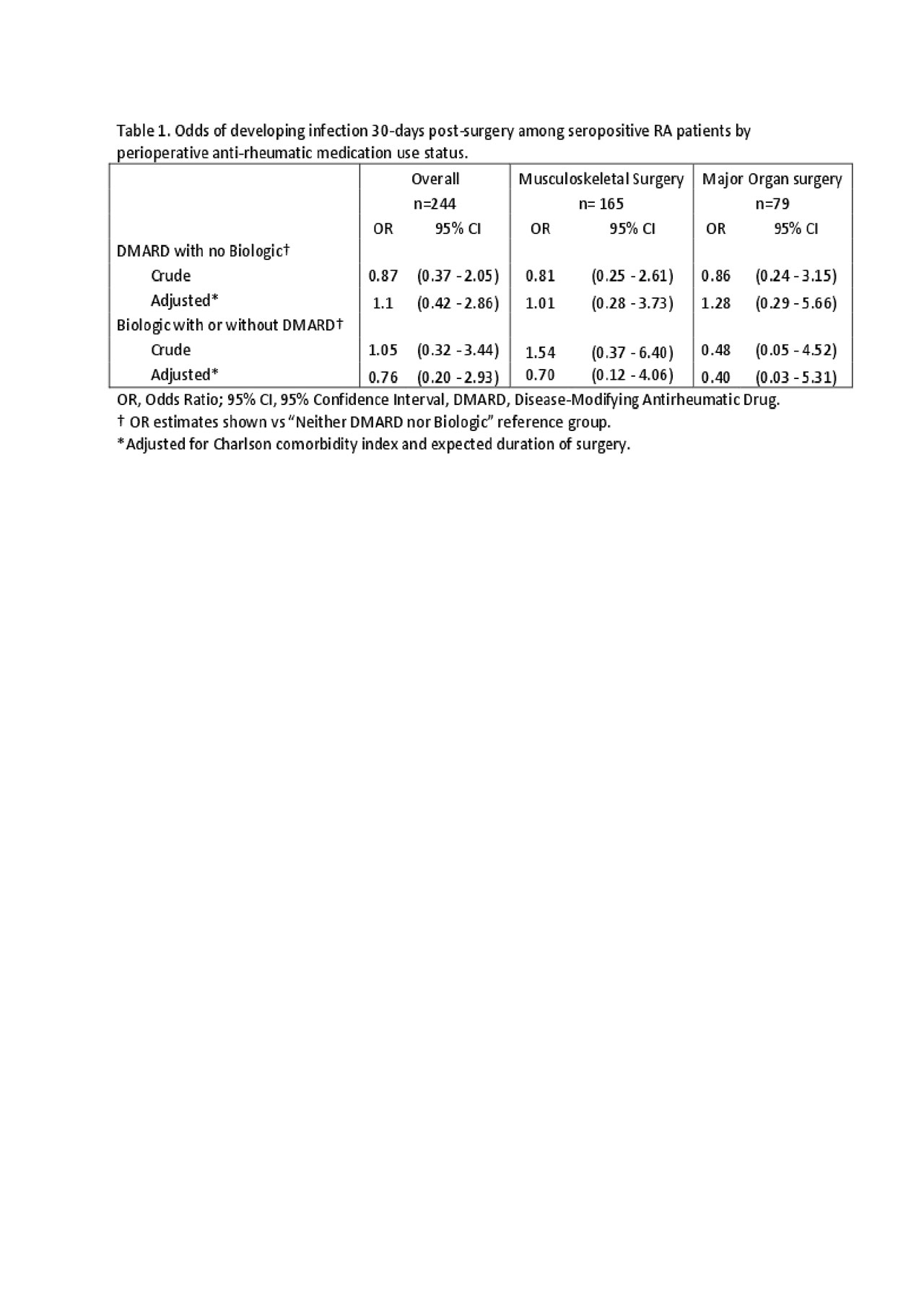
Results: 154 seropositive RA patients underwent 244 surgeries (165 musculoskeletal and 79 major organ). Patients were predominantly female (78%), white (94%), overweight or obese (73%) with a mean age of 62 years, and a mean Charlson comorbidity index of 2.3. Of the 244 surgeries, 116 (47.8%) were performed on no anti-rheumatic medications, 95 (39.1%) on a DMARD with no biologic, and 32 (13.2%) on a biologic with or without a DMARD. The groups were well-balanced on age, sex, race, baseline BMI, Charlson comorbidity index, surgery type, perioperative steroid use, antibiotic use and expected duration of surgery (p ≥ 0.1 for all comparisons). In total, 28 surgeries (11.5%) among 23 patients were complicated by a post-operative infection within 30 days: 14 (12%) in the no-medication group, 10 (11%) in the DMARD group, and 4 (13%) in the biologic group (p = 0.9). Of the other examined predictors, higher Charlson comorbidity index and longer expected duration of surgery were associated with infection (p < 0.05). After adjustment for these two predictors, overall and for musculoskeletal and major organ surgeries separately, perioperative use of anti-rheumatic drugs was not associated with increased odds of post-operative infection (table 1).
Conclusion: Perioperative use of anti-rheumatic medications was not associated with 30-day odds of post-operative infection in RA patients undergoing musculoskeletal or major organ surgery. Rather, higher Charlson comorbidity index and longer expected duration of surgery predicted postoperative infections in this RA population.
To cite this abstract in AMA style:
Kerski M, Boersma P, Miller E, Brenner A, Melton G, Shmagel A. Perioperative Anti-rheumatic Medications Are Not Associated with 30-day Odds of Infection in Rheumatoid Arthritis Patients Undergoing Surgery: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/perioperative-anti-rheumatic-medications-are-not-associated-with-30-day-odds-of-infection-in-rheumatoid-arthritis-patients-undergoing-surgery-a-retrospective-cohort-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perioperative-anti-rheumatic-medications-are-not-associated-with-30-day-odds-of-infection-in-rheumatoid-arthritis-patients-undergoing-surgery-a-retrospective-cohort-study/