Session Information
Date: Saturday, November 6, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster I (0387–0413)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Among the autoimmune rheumatic diseases, there is precedent for utilizing cutaneous manifestations of systemic disease as clues to clinical phenotype and disease prognosis. Though skin thickening affects >90% of patients with SSc, perifollicular hypopigmentation is observed less frequently. We sought to determine whether perifollicular hypopigmentation is associated with demographics, clinical features, and autoantibody profiles.
Methods: Data from SSc patients were prospectively collected from a single tertiary academic medical center. Patients were consecutively recruited, with additional targeted recruitment to enrich for patients with hypopigmentation. A standardized data collection form was completed on each patient including anatomic distribution of hypopigmentation. Autoantibody screens were performed using the commercially available Euroline immunoblot assay [Scleroderma Nucleoli Profile Uroline (IgG); Euroimmun, Lubeck, Germany]. Associations between perifollicular hypopigmentation and distinct features of SSc were assessed using logistic regression.
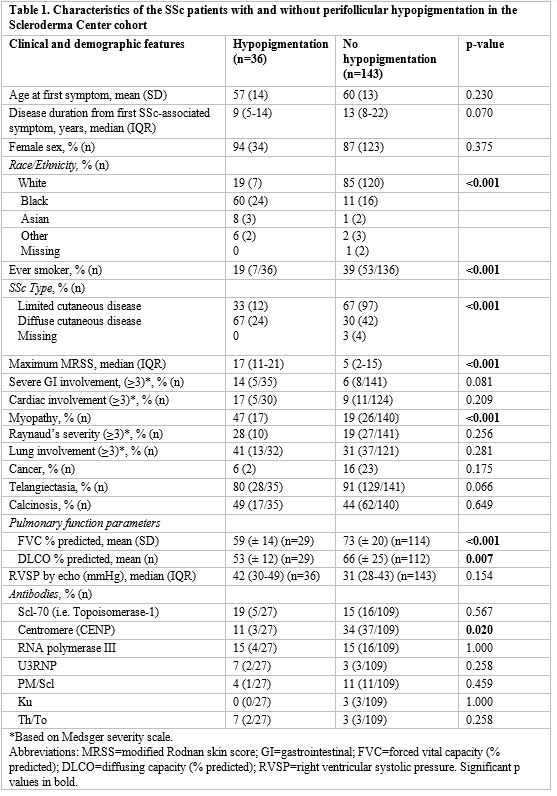
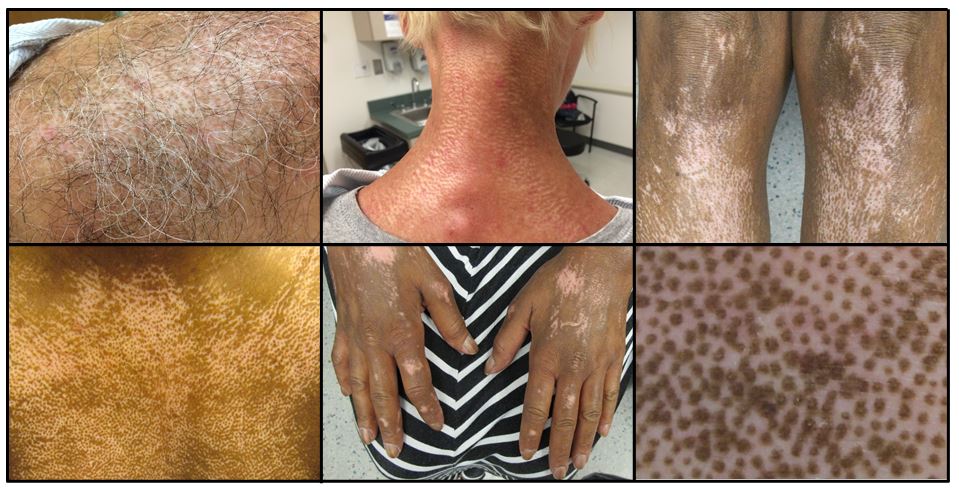
Results: Of the 179 adult SSc patients enrolled (Table 1), 36 (20%) SSc patients had perifollicular hypopigmentation. Among patients with perifollicular hypopigmentation, 94% (n=34) were female and 33% (n=12) had limited cutaneous SSc. Significant heterogeneity in the distribution of perifollicular hypopigmentation was observed, with dominant patterns involving the face/scalp (n=19), posterior neck (n=14), chest/back/leg (n=12/region), and dorsum hand (n=11) (Table 1). In univariable logistic regression analyses, black race (OR 15.63, 95% CI 6.6-37.20, p< 0.001), diffuse cutaneous disease (OR 4.62, 95% CI 2.11-10.09, p< 0.001), a higher maximum MRSS (OR 1.05, 95% CI 1.02-1.08, p=0.003), myopathy (OR 3.92, 95% CI 1.80-8.57, p< 0.001), a lower minimum FVC % predicted (OR 0.96, 95% CI 0.94-0.99, p=0.001), and a lower minimum DLCO % predicted (OR 0.97, 95% CI 0.95-0.99, p=0.009) were associated with perifollicular hypopigmentation (Table 2). An association with severe GI involvement (OR 2.77, 95% CI 0.85-9.07, p=0.09) trended towards significance. Anti-centromere antibodies inversely associated with perifollicular hypopigmentation (OR 0.24, 95% CI 0.07-0.86, p=0.028). In multivariable logistic regression analyses, diffuse cutaneous subtype (OR 4.28, 95% CI 1.46-12.53, p=0.008) was significantly associated with perifollicular hypopigmentation, even after adjusting for age, race, and disease duration. An association between perifollicular hypopigmentation and the presence of myopathy trended towards significance (OR 2.30, 95% CI 0.87-6.10, p=0.09).
Conclusion: Perifollicular hypopigmentation is observed in a subset of patients with SSc, and associates with diffuse cutaneous disease, black race, and myopathy. The distribution of perifollicular hypopigmentation is variable, with distinct patterns observed across patients. Larger longitudinal studies exploring whether specific patterns of perifollicular hypopigmentation associate with the development of internal organ complications may provide insight into patient risk stratification.
 39851957_1F2A_4BE5-946A-FB34AAB5729E.jpeg”
39851957_1F2A_4BE5-946A-FB34AAB5729E.jpeg”
 9D0C94FE-EB4C_46C3-821C-0EAA9569D553.jpeg”
9D0C94FE-EB4C_46C3-821C-0EAA9569D553.jpeg”
 52B9CEDD-758C_4142-953B-FB8ECD758852.jpeg”
52B9CEDD-758C_4142-953B-FB8ECD758852.jpeg”
To cite this abstract in AMA style:
Chung M, Perin J, Richardson C, Mecoli C, Wigley F, McMahan Z. Perifollicular Hypopigmentation in Systemic Sclerosis: Associations with Clinical Features and Internal Organ Involvement [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/perifollicular-hypopigmentation-in-systemic-sclerosis-associations-with-clinical-features-and-internal-organ-involvement/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perifollicular-hypopigmentation-in-systemic-sclerosis-associations-with-clinical-features-and-internal-organ-involvement/
