Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Cognitive impairment (CI) is a common neuropsychological manifestation of Systemic Lupus Erythematosus (SLE) with a prevalence of 38% [95% confidence interval: 33,43%]. Previous studies, have reported promising results on the utility of the Montreal Cognitive Assessment (MoCA) as a screening tool for CI in SLE compared to a comprehensive neuropsychological battery (CNB). The aim of this study was to assess the utility of the MoCA as a screening test for the detection of CI using a comprehensive NB as the gold standard for classification of cases.
Methods: From 2016 to 2019, 276 consecutive consenting adult SLE patients (excluding those with learning disabilities, and less than semi-fluent English language skills were administered the MoCA followed by a CNB. The MoCA, ranging from 0-30, was designed to screen for Mild Cognitive Impairment (MCI) in dementia a score of ≥26 considered above the threshold for MCI. In this study, patients were classified as having CI if they had a z-score of ≤-1.5 in ≥2 domains of the 6 domains of CNB, and otherwise non-CI. Descriptive statistics and two-by-two contingency tables with a MoCA cut-off score of 26 were applied to determine its sensitivity (Se) and specificity (Sp) to CI. The Se, Sp, positive predictive value (PPV) and negative predictive value (NPV) were evaluated. Additionally, a discriminant function analysis was applied to assess the ability of the MoCA to differentiate between CI, undetermined CI (one domain with a z-score of ≤-1.5) and non-CI patients.
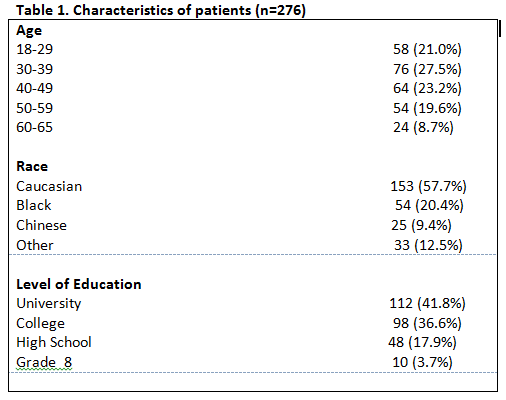
Results: 276 SLE patients were enrolled; 89.5% were females and the mean age was 41.2 ± 12.2 years at enrolment, and mean SLE duration of 14.1 ± 10.1 years (demographics in Table 1). Based on the CNB, 129 patients (47%) had CI, 85 (31%) had undetermined CI, and 62 (22%) were non-CI patients.
CI was not accurately predicted by MoCA with an area under curve (AUC) of 65% [95% Confidence interval: 0.59, 0.72]. The cut-off of 26 yielded Se, Sp, PPV and NPV of 50%, 70%, 59% and 61%, respectively.
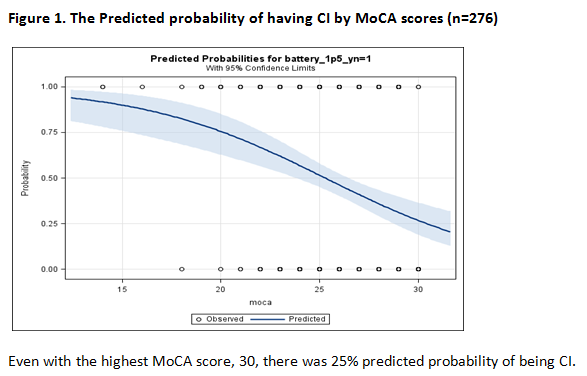
There was a 25% predicted probability of CI with the highest score (30) on the MoCA (Figure 1). Although the MoCA cut-off score of 27 reached a sensitivity of 80%, the specificity was very low at 45%.
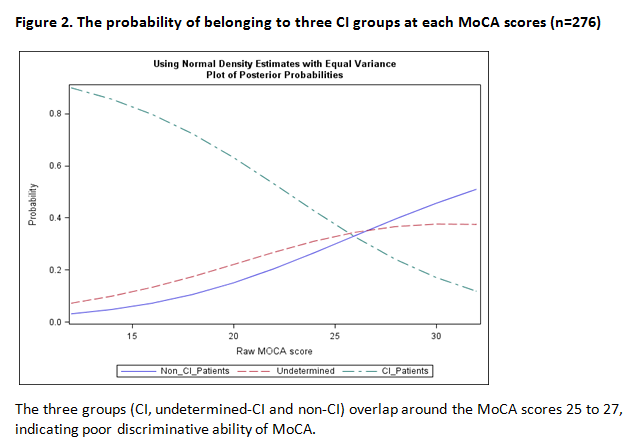
Based on the discriminant function analysis, the misclassification rates in the 3 categories (CI, undetermined-CI and non-CI) were 50%, 83%, and 44%, respectively. All three categories overlapped between the scores 25 to 27 (Figure 2). Thus, the MoCA had low ability to accurately identify CI status.
Conclusion: This analysis does not provide sufficient evidence to recommend MoCA as a screen for CI in SLE compared to a CNB. There was a low predicted probability of having CI with a low MoCA score and a relatively high predicted probability of having CI with a high MoCA score.
To cite this abstract in AMA style:
Kakvan M, Green R, Ruttan L, Tartaglia M, Wither J, Zandy M, Bonilla D, Choi M, Su J, Fritzler M, Beaton D, Touma Z. Performance of Montreal Cognitive Assessment (MoCA) in Screening for Cognitive Impairment in Patients with Lupus Compared to the Neuropsychological Battery [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/performance-of-montreal-cognitive-assessment-moca-in-screening-for-cognitive-impairment-in-patients-with-lupus-compared-to-the-neuropsychological-battery/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/performance-of-montreal-cognitive-assessment-moca-in-screening-for-cognitive-impairment-in-patients-with-lupus-compared-to-the-neuropsychological-battery/