Session Information
Date: Sunday, November 12, 2023
Title: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular disease (CVD) is a major cause of mortality in systemic lupus erythematosus (SLE). Role of conventional risk scores which predict cardiovascular events, to detect subclinical atherosclerosis in SLE is not established. In this study we assessed the performance of QRESEARCH database risk score-3 (QRISK3), Systemic COronary Risk Evaluation (SCORE), WHO (World Health Organization), Framingham (FRS) and modified Framingham(mFRS) CVD scores in subclinical atherosclerosis and determine clinical associations of the same
Methods: In this single centre cross-sectional analytical study, we enrolled 108 female SLE patients (without CVD) aged 40-60 years and 108 age matched healthy controls. Demography, disease activity, autoantibodies, steroid dose were noted. Subclinical atherosclerosis was defined by presence of either carotid plaque or abnormal carotid intima media thickness (cIMT) on ultrasound. CVD risk scores (QRISK3, SCORE, WHO, FRS and mFRS) were assessed. Agreement between scores was determined using kappa coefficient
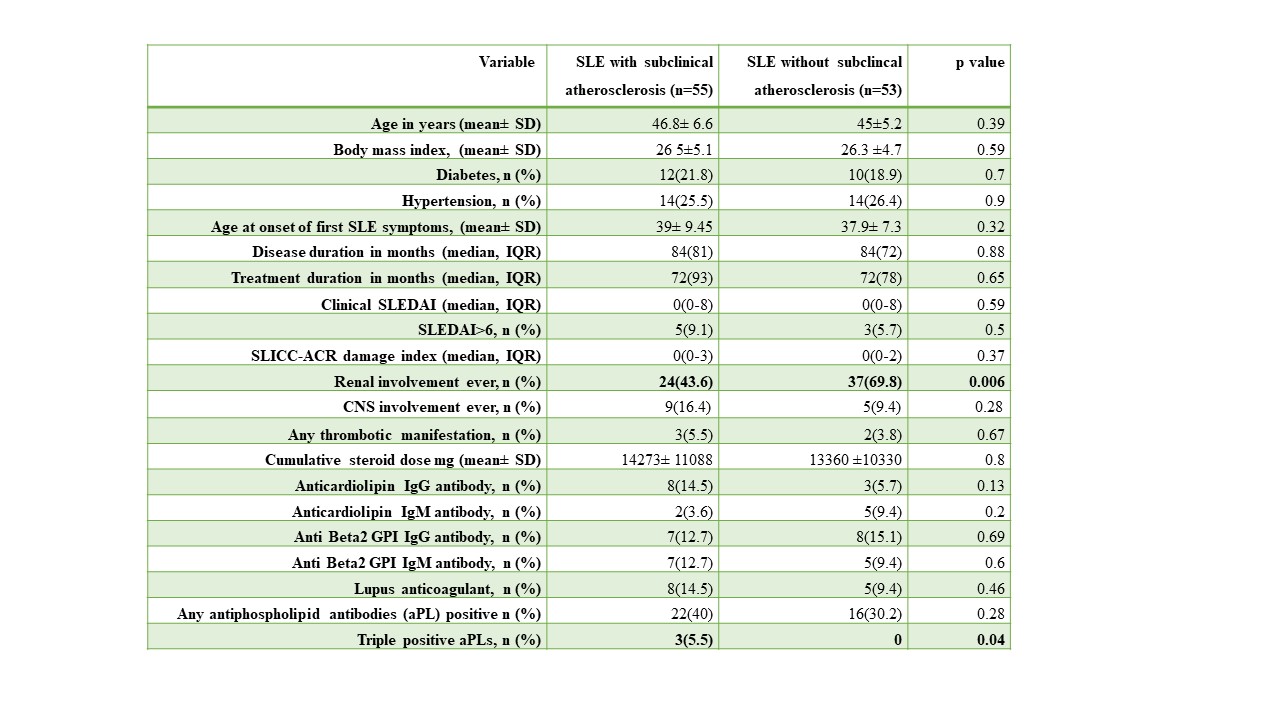
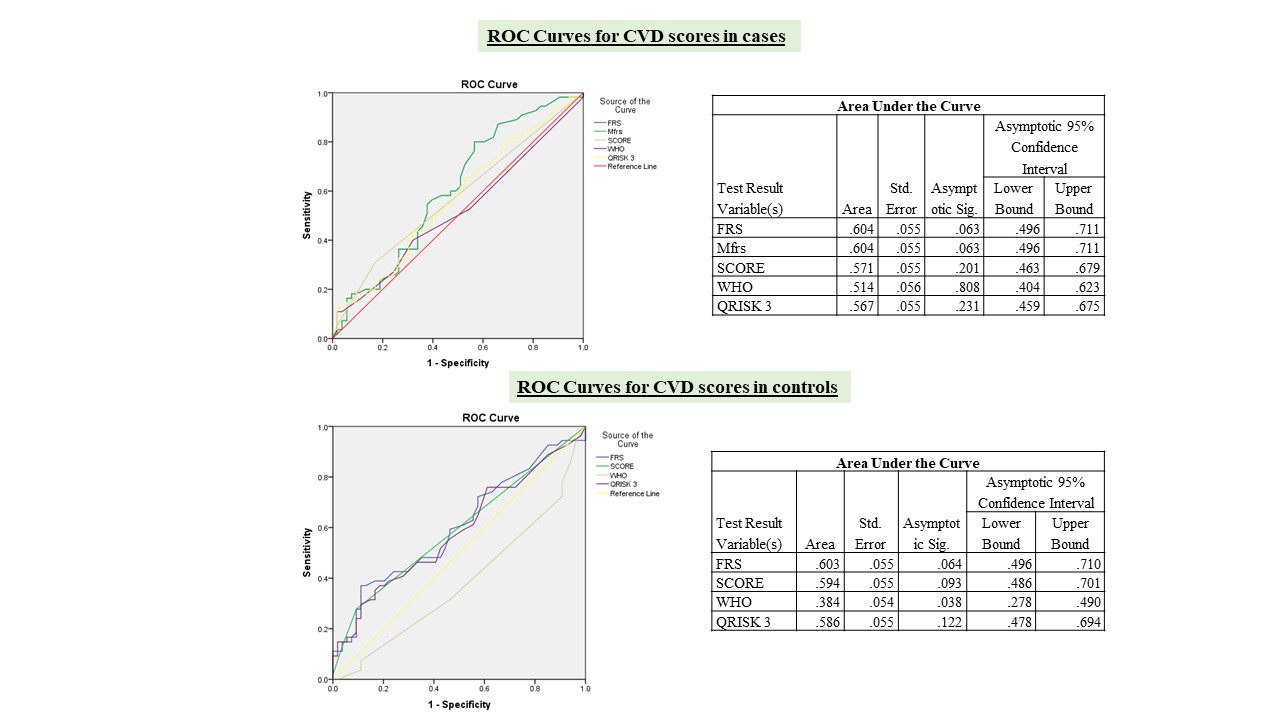
Results: Mean age of patients was 46±6 years, median duration of SLE was 72(93)months, median SLEDAI 0(0-8) and SLICC-ACR damage index was 0 (0-3) (Table 1).Subclinical atherosclerosis was present in 55 (51%) SLE [abnormal cIMT-44(41%) and plaque- 17(16%)] and in 52 (48%) controls [abnormal cIMT-46(42%) and plaque 12(11%)].Mean cIMT was comparable (0.62 ±0.2 cm) in cases and controls. All CVD risk scores had low sensitivity but good specificity to identify subclinical atherosclerosis in patients and controls (Table 2). Area under the curve (AUC) of the receiver operating characteristic curve (ROC), with subclinical atherosclerosis as outcome, showed that all scores had poor discriminatory capacity (Fig 1). In SLE, WHO and FRS had moderate agreement (kappa coefficient k 0.53), QRISK3 and mFRS had substantial agreement (k 0.65) with subclinical atherosclerosis, whereas in controls with FRS and QRISK3, and SCORE and WHO had substantial agreement (k 0.66 and 0.7 respectively) (Table 3). Proportion of patients having triple positive antiphospholipid antibodies were significantly higher in SLE with subclinical atherosclerosis than without (5.5% vs 0, p=0.04). Renal involvement was significantly less in SLE with subclinical atherosclerosis than without (43.6% vs 69.8%, p=0.006)
Conclusion: Prevalence of subclinical atherosclerosis was comparable in SLE and controls (51% vs 48%), though carotid plaques were significantly more prevalent in SLE (17% vs 11%). Sensitivity of conventional CVD scores in detecting subclinical atherosclerosis in SLE was poor. Hence, until further scores are validated, screening for subclinical atherosclerosis using carotid ultrasound should remain gold standard
Table 3: Agreement between the CVD risk scores measured with the Kappa coefficient
To cite this abstract in AMA style:
MS G, Gopal A, Mary Thabah M, Mariaselvam C, Singh j, Kavadichanda C. Performance of Conventional Cardiovascular Risk Scores in Identifying Subclinical Atherosclerosis in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/performance-of-conventional-cardiovascular-risk-scores-in-identifying-subclinical-atherosclerosis-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/performance-of-conventional-cardiovascular-risk-scores-in-identifying-subclinical-atherosclerosis-in-systemic-lupus-erythematosus/