Session Information
Date: Tuesday, November 9, 2021
Title: Patient Outcomes, Preferences, & Attitudes Poster IV: COVID-19 (1589–1613)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: The COVID-19 pandemic has triggered nationwide disruptions that limit opportunities for physical activity (PA). Addressing suboptimal levels of PA is important for disease management and reducing risk of comorbidities in patients with rheumatologic conditions. The objective of this cross-sectional study was to investigate the impact of the COVID-19 pandemic on PA levels of patients with rheumatologic disease and to examine characteristics associated with decreased PA that may inform future PA interventions.
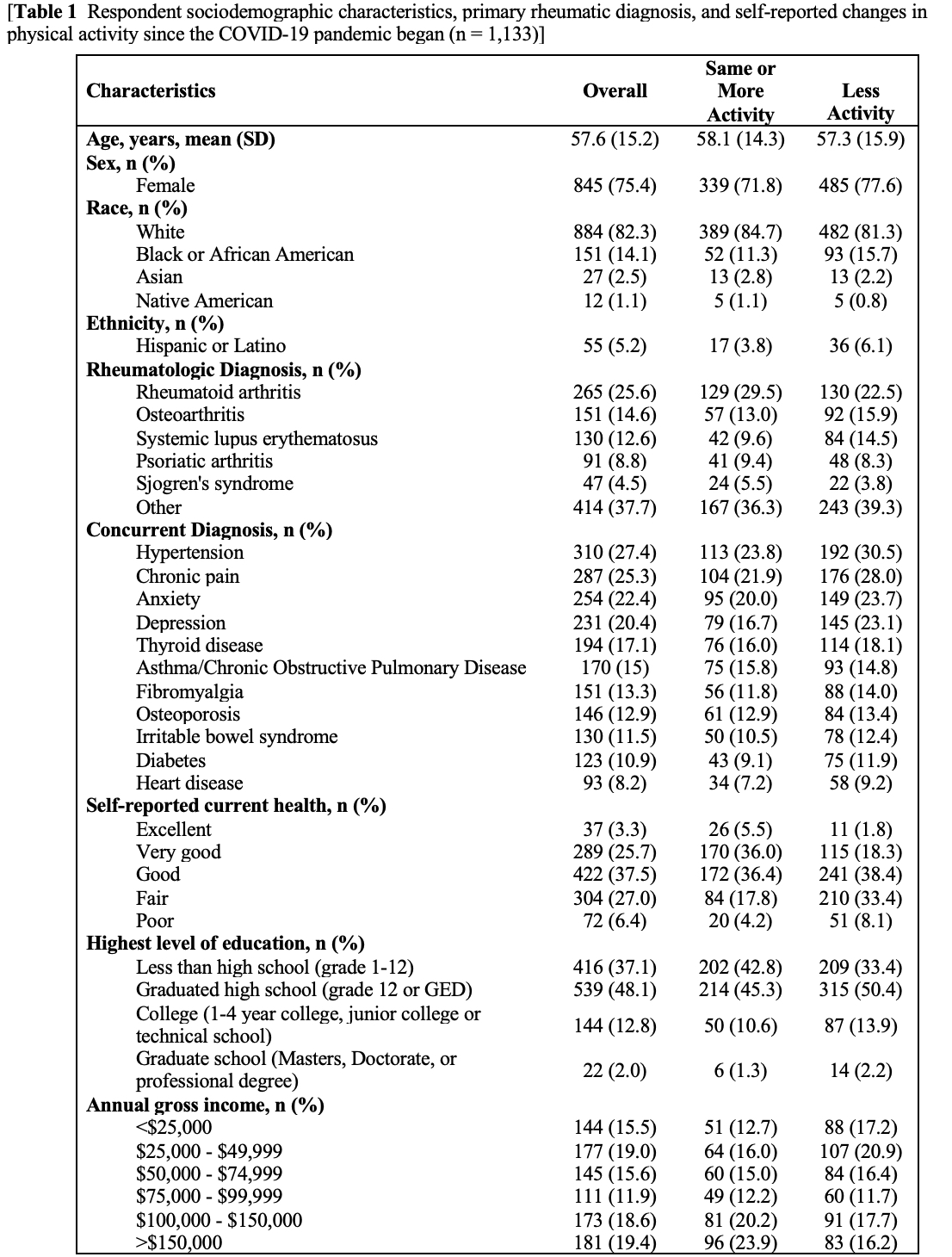
Methods: A convenience sample of adult patients with rheumatologic disease (n=7,776) were identified through electronic medical records from an academic healthcare system in North Carolina. Eligible patients were invited to participate in an online survey between July–September 2020. Rheumatologic and concurrent diagnoses as well as patient-reported outcomes during the COVID-19 pandemic were assessed, which included changes in PA, barriers to PA, psychological symptoms, and wellbeing. Descriptive statistics, age-adjusted odds ratios (OR), and 95% confidence intervals (CI) were computed to compare characteristics of those whose activity decreased versus those who did not (stayed the same or increased).
Results: A total of 1,133 participants completed the survey (17.2% response rate, mean age of sample: 57.6 ± 15.2 years, 75.4% female, 82.3% white and 14.1% African American). The most common primary diagnoses reported among participants include RA (25.6%), OA (14.6%), and SLE (12.6%). Over half of participants (55.5%) reported engaging in less PA since the start of the pandemic, followed by unchanged PA (26.6%) and increased PA (15.3%). Factors associated with engaging in less PA were male sex (OR 0.75, CI 0.57-0.99), lower income during the COVID-19 pandemic (OR 1.34, CI 1.01-1.79), and lower self-reported fair/poor health (OR 2.50, CI 1.91-3.27). Among rheumatologic diseases, a diagnosis of SLE was associated with lower self-reported PA (OR 1.59, CI 1.07-2.37). Comorbidities associated with decreased PA include chronic pain (OR 1.38, CI 1.04-1.82), depression (OR 1.48, CI 1.09-2.01), and hypertension (OR 1.44, CI 1.10-1.90). The most common reported barriers to PA include increased overall fear/anxiety (33.5%), lack of motivation (32.4%), and contracting coronavirus infection (32.1%). Most participants reported that they did not meet their exercise goals during the COVID-19 pandemic (67.2%).
Conclusion: The COVID-19 pandemic has further exacerbated barriers to PA in patients with rheumatologic diseases. There is a critical need to provide resources, support and multi-faceted to encourage PA in patients with rheumatologic diseases during the COVID-19 pandemic and beyond.
To cite this abstract in AMA style:
Dickson T, Englund T, McCormick E, Cleveland B, Allen K, Santana A, SaxenaBeem S, Walker J, Sheikh S. Perceived Impact of the COVID-19 Pandemic on Physical Activity Among Adult Patients with Rheumatologic Disease [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/perceived-impact-of-the-covid-19-pandemic-on-physical-activity-among-adult-patients-with-rheumatologic-disease/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perceived-impact-of-the-covid-19-pandemic-on-physical-activity-among-adult-patients-with-rheumatologic-disease/