Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Dignity is generally considered a fundamental feature of human individuals, related to human rationality and morality. This connotation of dignity is recognized as intrinsic dignity. However, in the clinical setting, the notion of dignity evokes how patients see themselves and are seen by others and how the nature of the illness in question affects the person’s life and identity. Perceived dignity is a recognized source of multifaceted distress in cancer patients, which has been associated with the medical care environment, and patients feel a diminished sense of worth or value and a burden to others. The spectrum of rheumatic diseases’ clinical expression provides evidence that a significant percentage of the patients might present with progressive health decline, disability, distressing symptoms affecting their capacity to continue with usual activities and roles, and limited autonomy, all of which threaten patients’ perceived dignity.
The study’s primary objective was to determine distress related to perceived dignity (DPD) among Mexican patients with RMDs. The rationale and methods for adapting and validating the Mexican version of the Patient Dignity Inventory (PDI-Mx) in the population are additionally described.
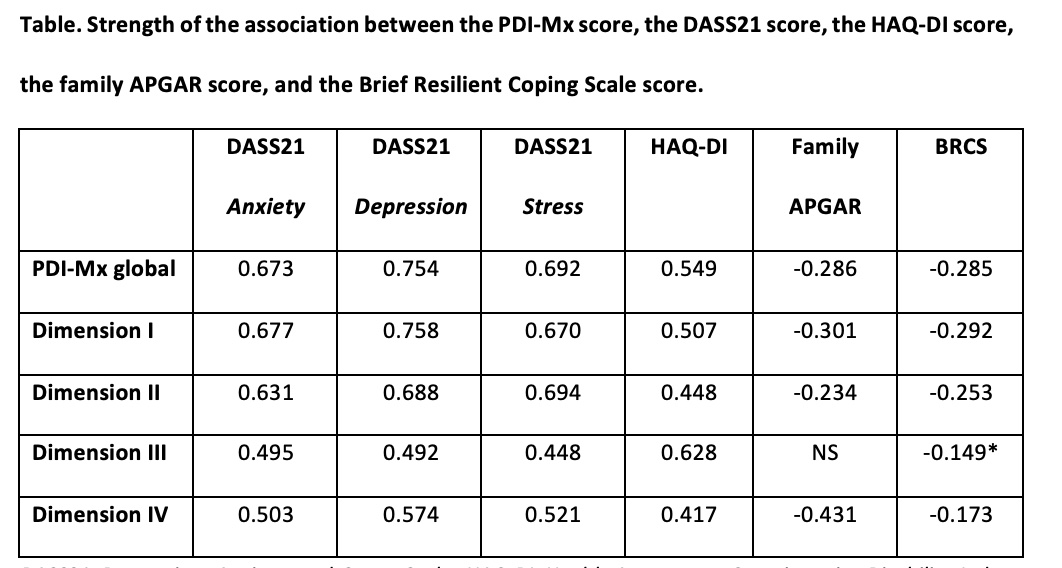
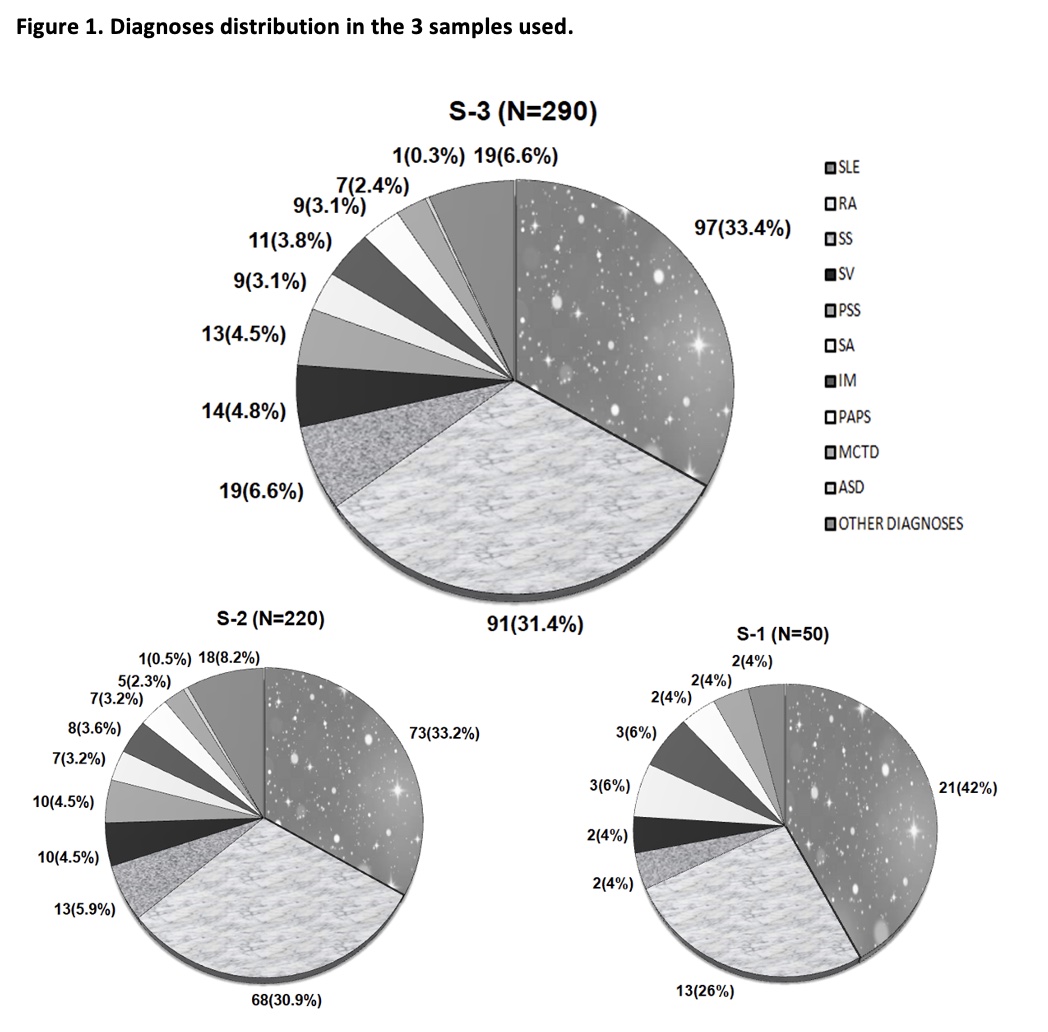
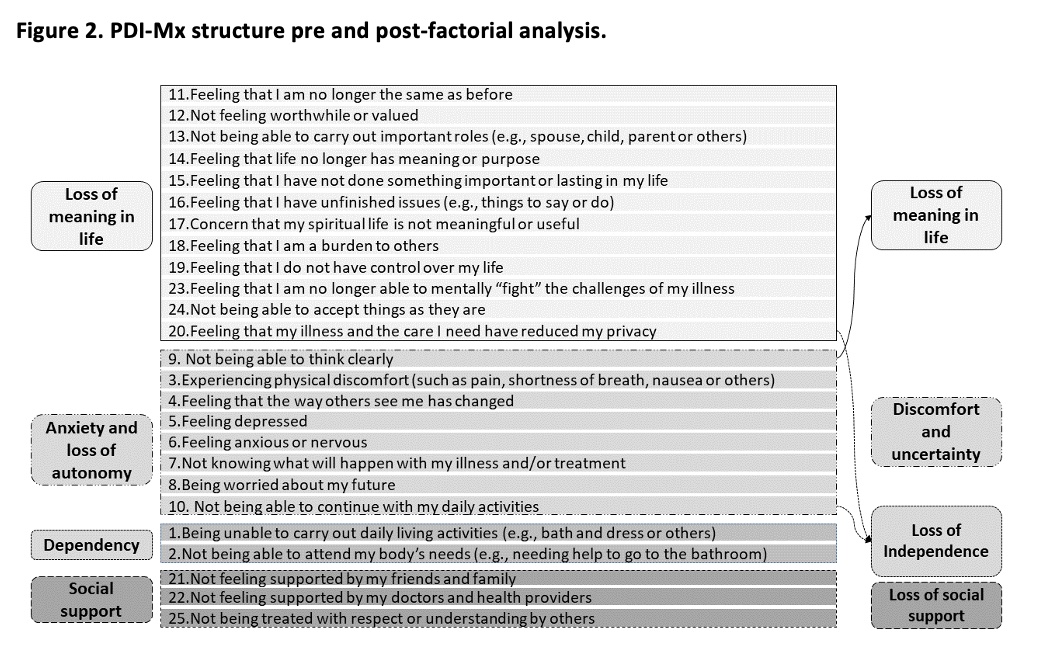
Methods: This cross-sectional study was developed in 2 phases (January 2022-July 2022). Three convenience samples of different patients were used, and quotes were considered to represent the ten most frequent local RMDs-related diagnoses (Figure 1). Phase 1 consisted of pilot testing and questionnaire feasibility (n=50 patients, Sample 1), and the PDI-Mx content validity (judgment experts’ agreement), construct validity (exploratory factor analysis), criterion validity (Spearman correlations), and reliability (internal consistency and temporal stability) in 220 outpatients (Sample 2), among whom 30 underwent test-retest. Phase 2 consisted of DPD quantification in 290 outpatients with RMDs (Sample 3). Receiving Operating Curve was used to define the best PDI-Mx cut-off for DPD (≥54.5, min-max:25-125, higher scores indicating more DPD) with the gold standard defined according to DASS21 scores of at least moderate severity for anxiety and depression and a psychiatric interview that confirmed clinically relevant symptoms of emotional distress.
Results: Overall, patients were representative of typical outpatients with RMDs from a National tertiary care level center, and the most frequent diagnoses were Systemic Lupus Erythematosus and Rheumatoid arthritis (Figure 1). DPD was present in 78 patients (26.9%). The 25-item PDI-Mx was found feasible, valid (experts’ agreement ≥82%; a 4-factor structure accounted for 68.7% of the total variance; moderate to high correlations between the PDI-Mx and questionnaires summarized in the Table) and reliable (Cronbach’s ɑ=0.962, ICC=0.939 [95%CI=0.913-0.961]). The structure of the PDI-Mx underwent mild modifications after factorial analysis (Figure 2).
Conclusion: DPD was homogeneously present in up to 27% of Mexican patients with different RMDs. The PDI-Mx process validation was rigorous, and its critical quality indicators were validity, reliability, and feasibility.
To cite this abstract in AMA style:
Pascual Ramos V, Guaracha Basañez G, Contreras Yañez I, Cuevas Montoya M, Rodríguez Mayoral O, Chochinov H, García Alanís M. Perceived Dignity in Patients with Rheumatic Diseases: An Unrecognized Source of Emotional Distress [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/perceived-dignity-in-patients-with-rheumatic-diseases-an-unrecognized-source-of-emotional-distress/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perceived-dignity-in-patients-with-rheumatic-diseases-an-unrecognized-source-of-emotional-distress/