Session Information
Date: Tuesday, November 14, 2023
Title: (1945–1972) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Dermatomyositis (DM) is a relatively rare condition with significant morbidity and mortality across the lifespan.Recent advances in diagnostics and therapeutics have significant potential to improve outcomes.We set up the Penn State Registry of Inflammatory Myopathies (PRIMO) and sought to understand the current status of DM patients seen in the relatively rural population of south-central Pennsylvania.Objectives are to determine whether our patients have had access to optimal care and to explore approaches to improving outcomes.
Methods: Records for patients seen at Hershey Medical Center with diagnosis code M33 (including all subcodes) in a 10 year period starting 1/1/2010 were extracted from the EMR.Each record was reviewed (by JC) to confirm the 2017 EULAR/ACR classification criteria for idiopathic inflammatory myopathies. Features of108 patients with DM or juvenile DM were reviewed in detail (by JC and KR) using data extraction forms and compiled in a REDCap database.Descriptive statistics were used to summarize results.
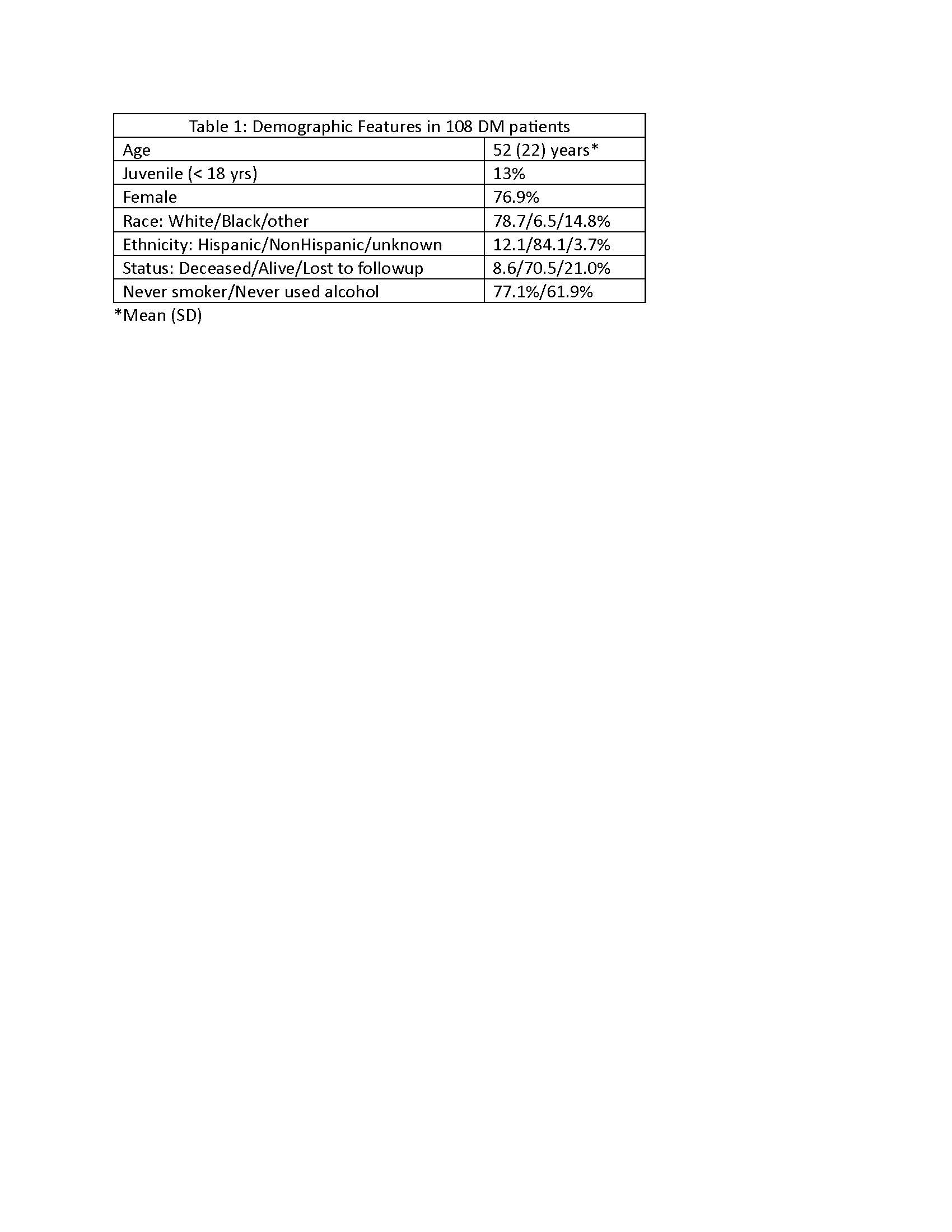
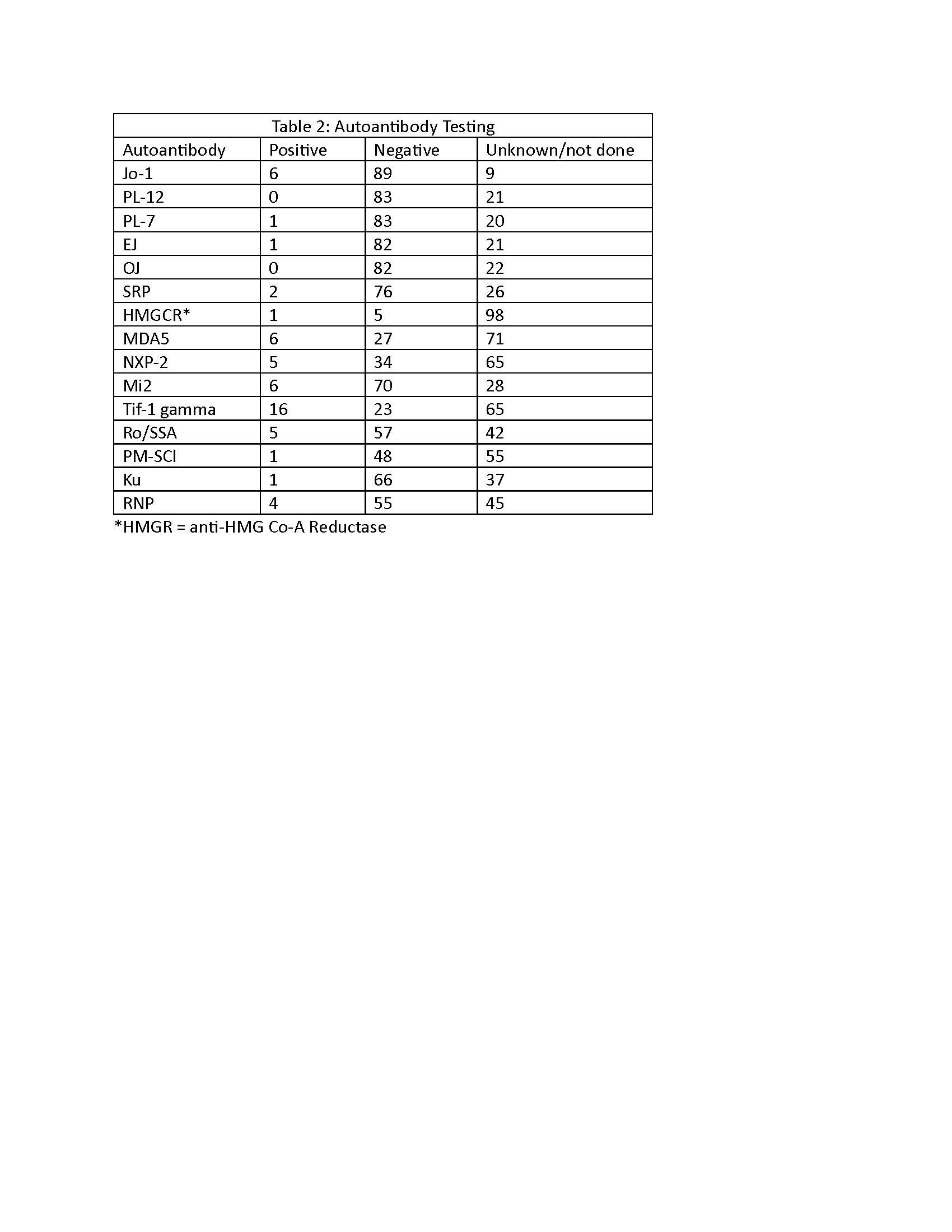
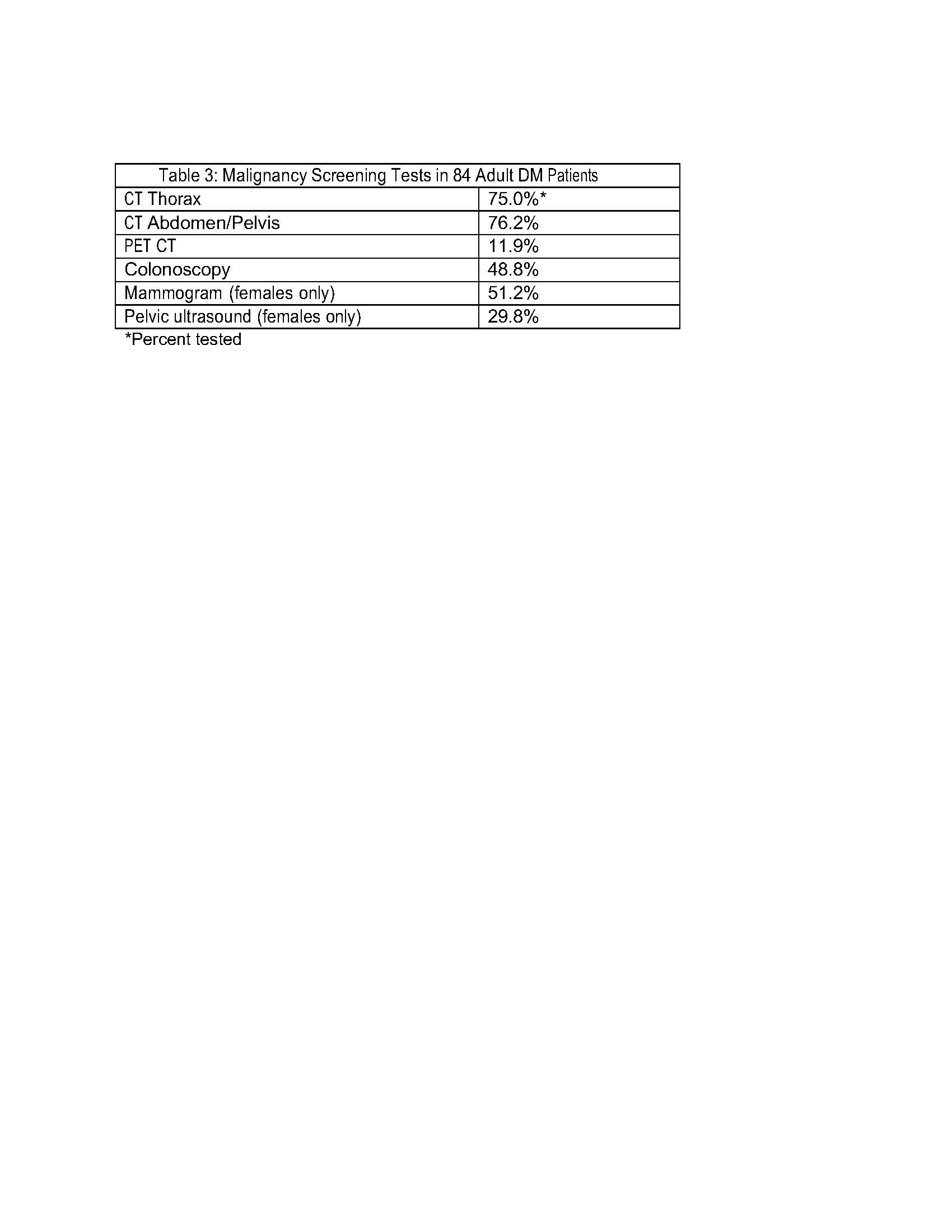
Results: Most patients (87%) had adult DM; the overall average age was 52 years (range 7 to 88 years).Other demographic features are shown (Table 1).Encounters for the first myositis-related symptoms occurred most commonly in family medicine (44%), dermatology (16.7%) and pediatrics (13.1%); only 6% had an initial myositis-related encounter in rheumatology.Common presenting symptoms were rash (94.2%) and muscle weakness (81.7%).Autoimmune comorbidities included celiac disease (14.3%) and thyroid conditions (28.4%).Familial conditions included RA (35.7%), SLE (21.4%) and Sjogren’s (14.3%); no patient reported a family history of DM or polymyositis.Lab testing at presentation showed elevated muscle enzymes (CK, LDH or transaminases) in 72% and ANA positivity in 66%; 2/3 had speckled pattern.Of myositis-specific autoantibodies (MSA) measured, the most prevalent was Tif-1 gamma, positive in 15.4% of those tested (Table 2).When performed, tissue biopsies were highly diagnostic (skin:43/49 patients tested, 88% positive; muscle 38/42, 90%).Muscle MRI done in 33 individuals showed inflammation in 73% and atrophy in 9%.Prevalence of malignancy (9.6%) was relatively low; screening for malignancies was not recorded for all patients (Table 3).Other testing for comorbidities included echocardiograms, which were normal in 88% of 25 examined and HRCT which showed ILD changes in 38% of 21 tested. Less than half of individuals had PFTs completed.
Conclusion: DM outcomes may be improving in part due to improved screening for comorbidities as well as availability of new treatment options.The rate of malignancy in our patients was lower than expected, despite the high prevalence of malignancy-related autoantibodies (TIF-1g, NXP-2) among those patients with evaluation for MSA. Whether this is related to length of followup is being further investigated.Our study also demonstrates that screening for comorbidities had lower than expected utilization representing a potential practice gap.Future studies are needed to determine if this a local trend, or a population shortfall in DM management. Development of personalized medicine approaches should be prioritized.
To cite this abstract in AMA style:
Colello J, Riggle K, Foulke G, Newman P, Carter J, Olsen N. Penn State Registry of Inflammatory Myopathies (PRIMO) Provides Insights into Disease Features and Co-Morbidity Screening Utilization [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/penn-state-registry-of-inflammatory-myopathies-primo-provides-insights-into-disease-features-and-co-morbidity-screening-utilization/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/penn-state-registry-of-inflammatory-myopathies-primo-provides-insights-into-disease-features-and-co-morbidity-screening-utilization/