Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Antiphospholipid syndrome (APS) is an autoimmune condition defined as the presence of thrombotic events and/or pregnancy morbidity, accompanied by persistent antiphospholipid antibodies (aPLs). Pediatric APS is rare, often severe, and usually occurs in conjunction with systemic lupus erythematosus (SLE). There currently are no pediatric specific diagnostic or classification criteria for APS. This study aims to describe the characteristics of children with APS in a large tertiary care center.
Methods: With approval from our Institutional Review Board, retrospective descriptive study of patients diagnosed with APS from 2012 to 2025 was performed. The cohort was further stratified into primary APS and secondary APS. Demographic, clinical manifestations, serologies, and treatments were compared between groups. Threshold criteria were defined utilizing the 2023 ACR/EULAR Antiphospholipid Syndrome Classification Criteria threshold of >40 units for moderate/high titer. Statistical analysis for significance was calculated utilizing Fischer exact test.
Results: Thirty-nine patients were included in the study, 16 (41%) with primary APS and 23 (59%) with secondary APS. Most patients with secondary APS had a diagnosis of SLE and 3 patients with primary APS later developed SLE. Hematologic manifestations were more common in secondary APS. Arterial thrombosis most commonly presented as a stroke. Catastrophic antiphospholipid syndrome (CAPS) was identified in 18% of all patients, all of whom survived. Ten patients with LA hypoprothrombinemia syndrome (LAHPS) were identified, only 1 of whom had APS. Four (10%) patients had aPL below criteria threshold with negative LA, while 5 (13%) had low titer aPL with positive LA. Persistent positivity was observed in 62% of all APS but only 26% were persistent above threshold. Persistence was statistically more common in the primary APS group; however, above threshold persistence only approached statistical significance. Triple positivity was mostly seen at criteria levels, with only 3 patients having triple positivity at low titers. Anticoagulant treatment was overall similar between the two groups, with heparin-based being most common. While patients with secondary APS received more immunomodulatory therapies, many primary APS patients did receive immunosuppressants, particularly rituximab. Two of the 6 who received rituximab were at the time of progression from primary APS to SLE.
Conclusion: Pediatric APS presents heterogeneously and with severe manifestations. Neurologic manifestations, a non-criteria manifestation, were common in this cohort, as was CAPS. Statistically significant differences between clinical and laboratory manifestations in primary and secondary APS were limited, possibly due to small sample size. Despite the small sample size, this high frequency of severe manifestations suggests APS may be underrecognized in milder cases. About a third of our patients fulfilled the threshold of aPL positive as defined by the most recent classification criteria for APS. This highlights the need for large-scale retrospective and prospective studies to address this definition in pediatric patients.
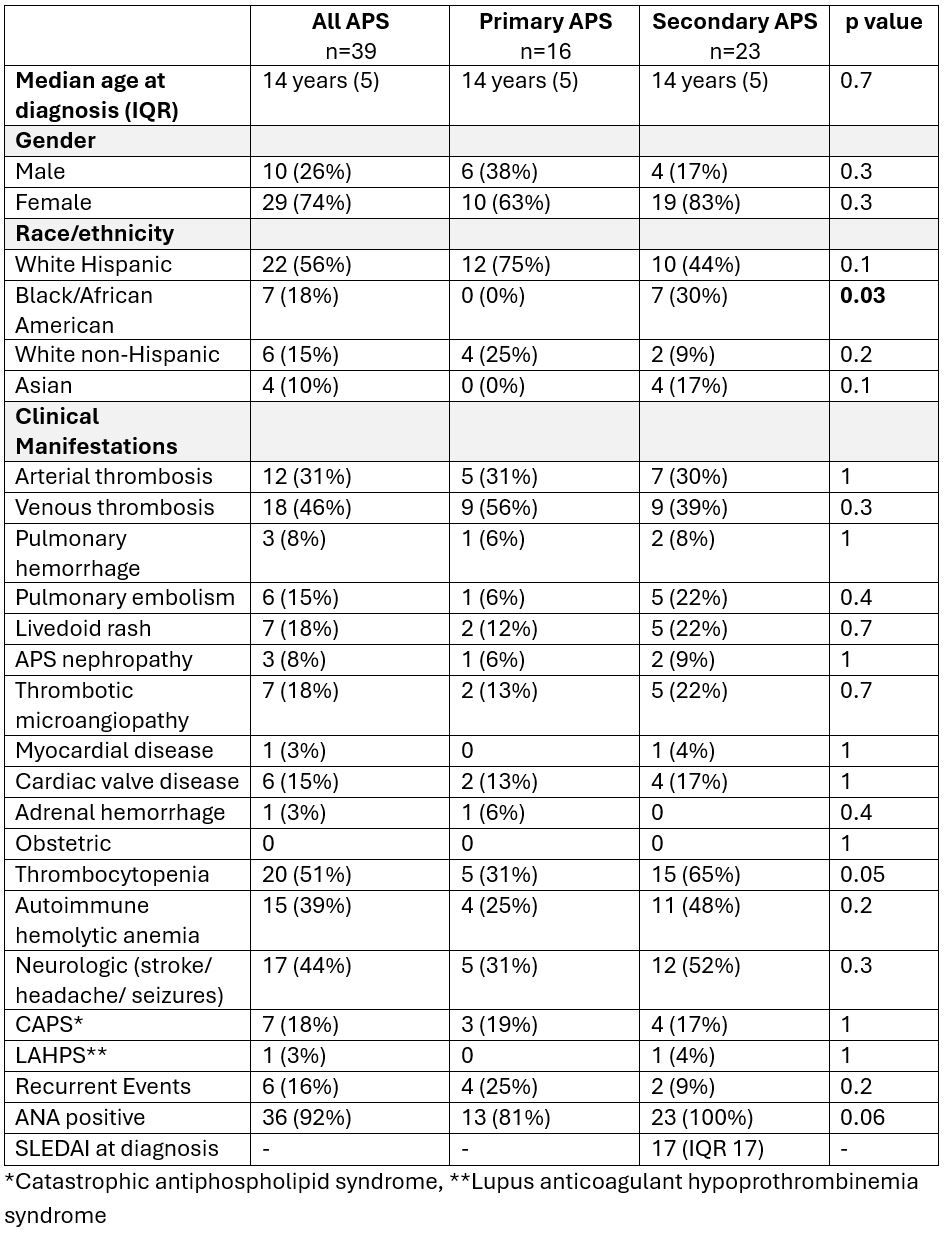 Table 1 Demographics and clinical manifestations
Table 1 Demographics and clinical manifestations
.jpg) Table 2 Laboratory manifestations
Table 2 Laboratory manifestations
To cite this abstract in AMA style:
Elrefai R, De Guzman M, Teruya J, Kostousov V, Navaei A, Kwan O. Pediatric Antiphospholipid Syndrome in a Large Tertiary Center [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/pediatric-antiphospholipid-syndrome-in-a-large-tertiary-center/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pediatric-antiphospholipid-syndrome-in-a-large-tertiary-center/

.jpg)