Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Session Type: Poster Breakout Session
Session Time: 5:10PM-5:40PM
Background/Purpose: Pediatric antiphospholipid syndrome (APS) is a thromboinflammatory disease classically defined by the presence of circulating antiphospholipid antibodies and either thrombotic events or pregnancy morbidity. Despite its potential to cause significant morbidity in children, pediatric APS is an understudied condition that lacks classification criteria specific to the pediatric age group. The objective of this study was to review our institution’s experience with pediatric APS in pursuit of a better understanding of the characteristics and treatment of children with APS.
Methods: We conducted a 20-year retrospective review of pediatric APS at a tertiary referral center. The electronic medical record system was queried for patients aged 21 and younger with a diagnosis of APS from 2000 through 2019. Fifty cases were evaluated further, and 22 were ultimately included in this study. Included cases were assessed for clinical and laboratory features, therapeutic management, and outcome data. Excluded cases failed to meet the revised Sapporo Classification criteria by age 18 or younger.
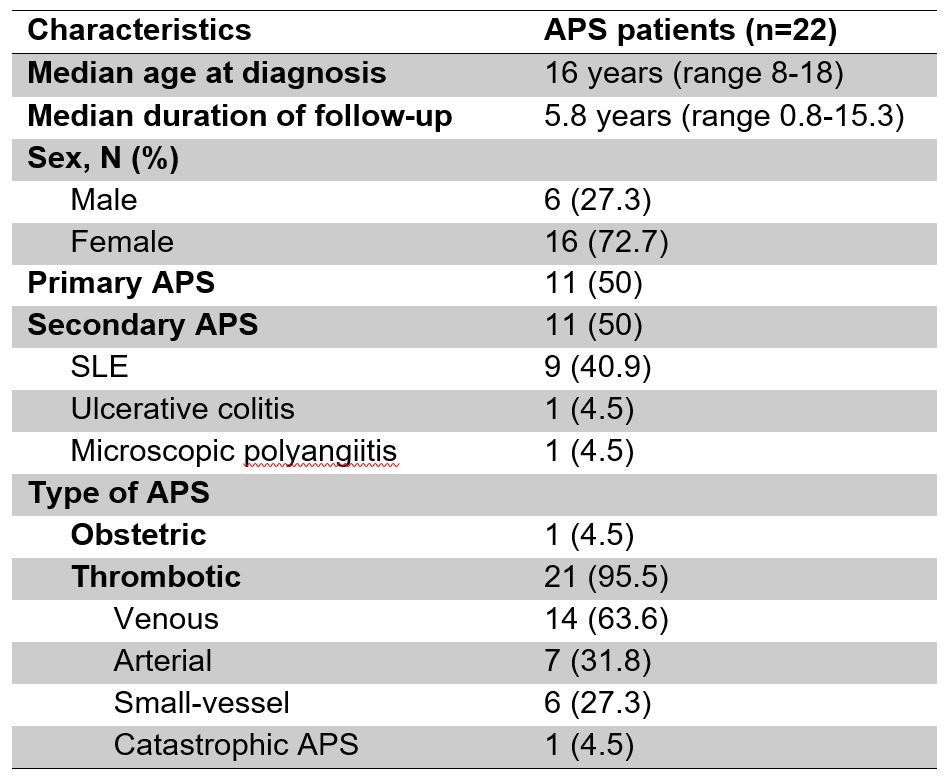
Results: Twenty-two patients were included with a median age at diagnosis of 16 years and median follow-up of 5.8 years (Table 1). Almost three-quarters of patients were female, and there were equal numbers of patients with primary and secondary APS (Table 1). Not surprisingly, secondary APS was primarily diagnosed in the context of SLE (9/11 cases). Regarding laboratory features, patients had durably positive anti-beta-2-glycoprotein I antibodies in 68% of cases, anticardiolipin antibodies in 82%, and lupus anticoagulant in 55%. A majority of patients tested were also positive for ANA, anti-double-stranded DNA, and anti-chromatin antibodies (Table 2). Two patients were tested for anti-phosphatidylserine/prothrombin antibodies, and both were positive. With regards to clinical features, 1 patient had obstetric APS and 21 patients had thrombotic APS (Table 1). Many patients had so-called “non-criteria” manifestations of APS, with thrombocytopenia, autoimmune hemolytic anemia, and livedo reticularis/racemosa especially common (Table 3). Although 2 patients were treated with aspirin alone, the majority (86%) received anticoagulation with warfarin or heparin products; 41% (9/22) were treated with both aspirin and anticoagulation. Direct oral anticoagulants and fondaparinux were used in four patients each at some point in their course. Analysis is ongoing to evaluate whether any particular approach to therapy was more or less effective, as well as whether patients with primary and secondary APS responded differently to treatment.
Conclusion: This is the largest case series to date of pediatric APS in a United States population, and thereby provides important context regarding potential phenotypes displayed by children with APS. There was a high prevalence of both non-criteria clinical manifestations and positivity of other autoimmune laboratory studies (for example, anti-chromatin antibodies), highlighting the need to consider these additional characteristics when developing pediatric-specific classification criteria and, most importantly, when considering this rare diagnosis in pediatric practice.
To cite this abstract in AMA style:
Madison J, Knight J. Pediatric Antiphospholipid Syndrome: Clinical Features and Therapeutic Interventions in a Series of 22 Cases [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/pediatric-antiphospholipid-syndrome-clinical-features-and-therapeutic-interventions-in-a-series-of-22-cases/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pediatric-antiphospholipid-syndrome-clinical-features-and-therapeutic-interventions-in-a-series-of-22-cases/