Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with SLE often have concomitant FM or symptoms similar to FM, including chronic pain, fatigue, sleep disturbance, and/or depression, potentially distinct from immune-mediated disease activity and comprising type 2 SLE symptoms. FM studies vary by included FM disease states and patient-reported outcomes (PROs), making comparability challenging. This study explored patterns of symptoms using Patient-Reported Outcomes Measurement Information System (PROMIS) measures that could provide richer information than 2016 ACR FM criteria for disease characterization and management in patients with SLE and other pain conditions.
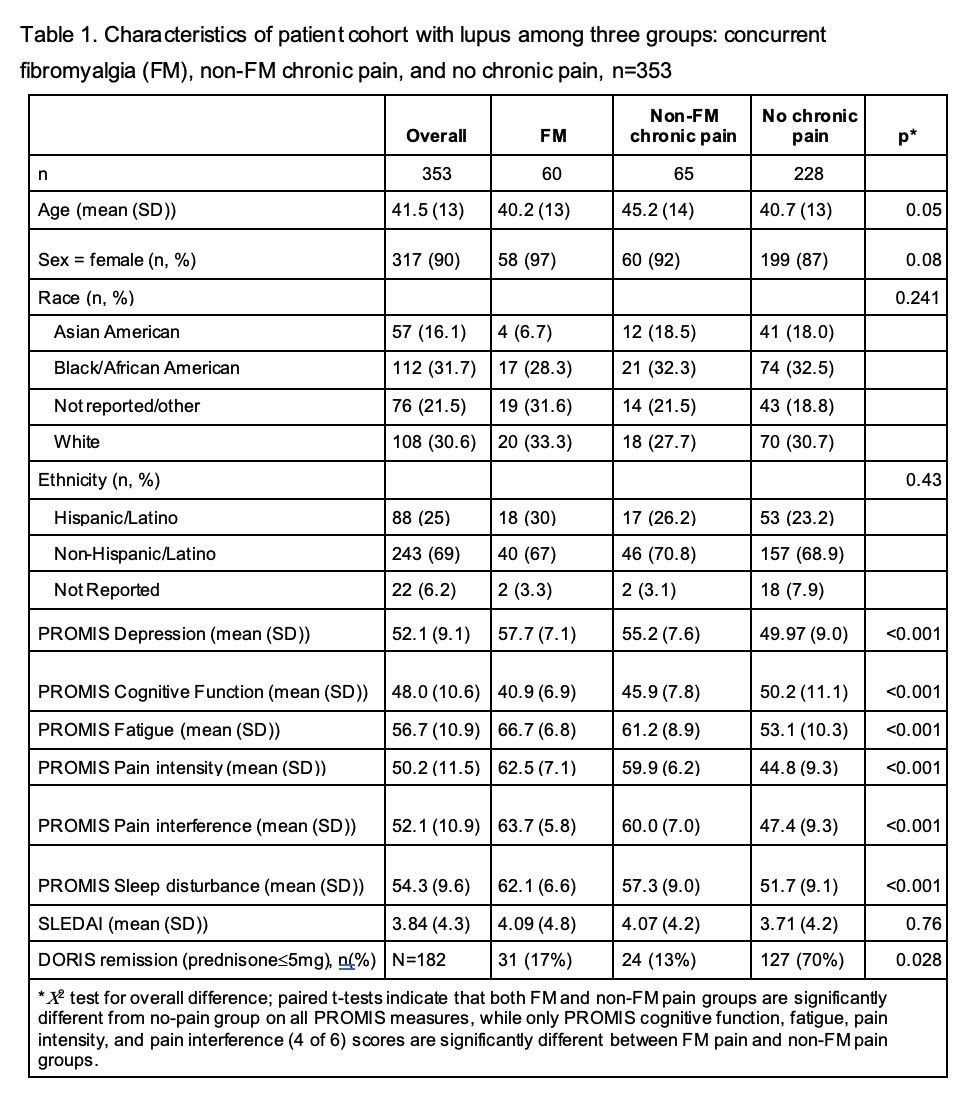
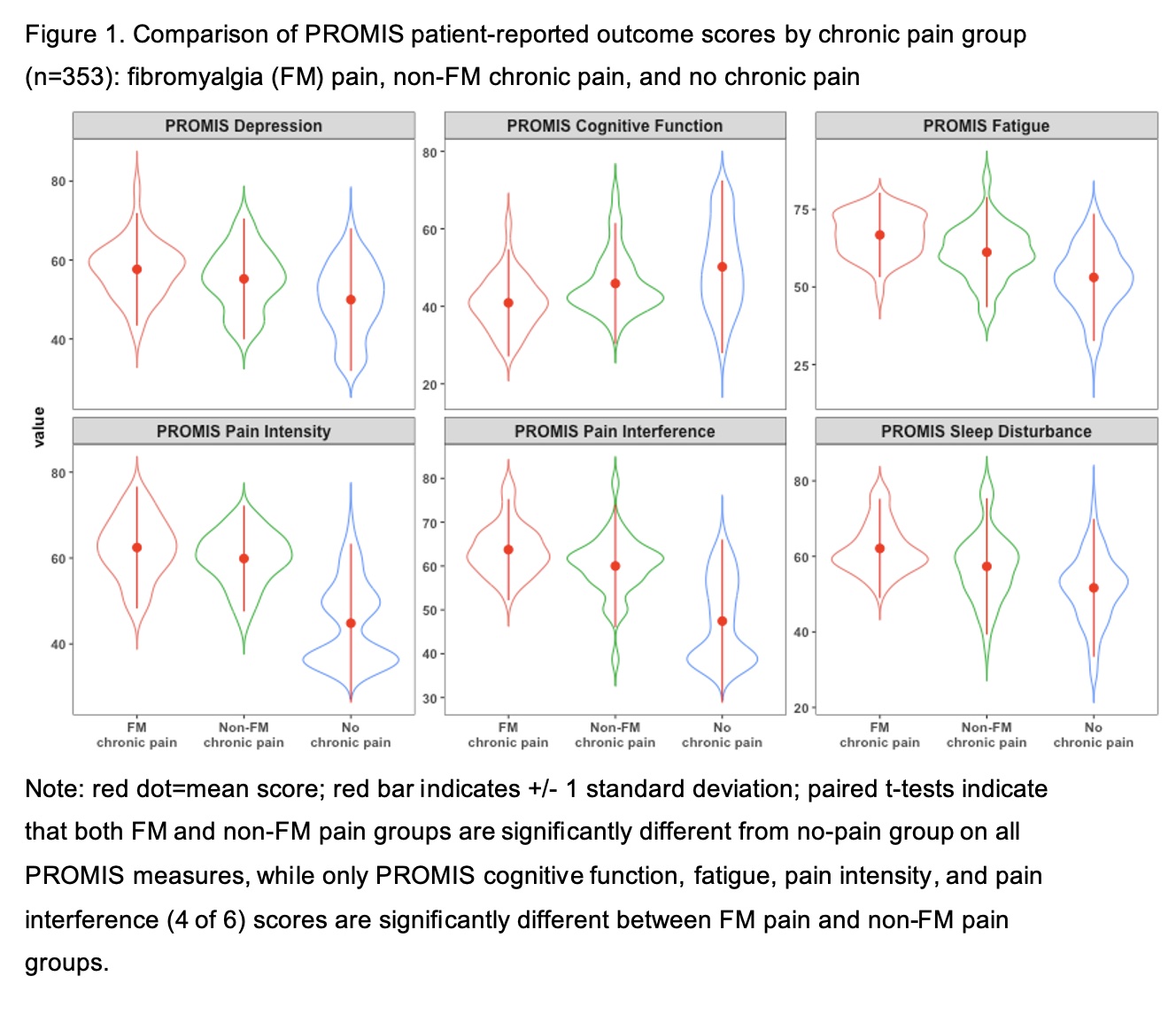
Methods: We categorized 353 patients with SLE into three groups based on responses to the FM Criteria Survey: 1) concurrent FM chronic pain, 2) concurrent non-FM chronic pain, and 3) no chronic pain. Based on specific PROs assessed in the FM Criteria Survey, we captured comparable PROMIS measures (i.e., depression, fatigue, pain, sleep, and cognitive function). We collected demographics and SLEDAI scores (categorized as < 4,4-7,8-12, >12). Comparisons by pain group used chi-squared tests and two-sample and paired t-tests unadjusted for multiplicity. Violin plots visualized differences.
Results: Thirty-five percent of patients (n=125) had chronic pain – approximately half with FM chronic pain (n=60) and half with non-FM chronic pain (n=65) – while 65% had no chronic pain (n=228). (Table 1) Mean PROMIS scores for fatigue, sleep disturbance, cognitive function, and depression were significantly different (p< 0.001) by pain group, with pain groups significantly different from the no-pain group (p< 0.01), and significant differences on 4 PROMIS measures (cognitive function, fatigue, pain intensity, and pain interference) between FM pain and non-FM pain groups (p< 0.02). The FM group consistently had worse mean symptom and function scores, the non-FM chronic pain group intermediate, and the no-chronic-pain group had best mean scores (i.e, lower symptoms and higher function). Strikingly, among the wide range of disease activity represented by SLEDAI, there was no significant association by pain group (p=0.76). There were no significant differences in demographics, except slightly higher age for non-FM chronic pain (p=0.05).
Conclusion: This study revealed that SLE patients with non-FM chronic pain also have symptoms in common with FM, such as fatigue, sleep disturbance, and cognitive issues, more often than SLE patients without chronic pain; however, symptoms are not as severe as those meeting FM criteria. Further, SLEDAI scores were not significantly different across groups. We propose PROMIS measures as an appropriate tool to gauge Type 2 SLE symptoms because they show more variation between SLE patients with and without FM. Different underlying pathophysiology may explain symptoms, important for future treatment studies.
To cite this abstract in AMA style:
Gold H, Li Y, Anthopolos R, Izmirly P, Buyon J, Masson M, Cohen B, Barbour K, Saxena A, Belmont H, Tseng C, Corbitt K. Patterns of Patient-reported Outcome Measures in Patients with Systemic Lupus Erythematosus with or Without Concurrent Fibromyalgia [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/patterns-of-patient-reported-outcome-measures-in-patients-with-systemic-lupus-erythematosus-with-or-without-concurrent-fibromyalgia/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patterns-of-patient-reported-outcome-measures-in-patients-with-systemic-lupus-erythematosus-with-or-without-concurrent-fibromyalgia/