Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Medication access and adherence are important issues in determining patient outcomes. We investigated sociodemographic factors and disparities associated with prescription medication access in a population-based cohort of lupus patients and controls.
Methods: Detailed data on prescription access and sociodemographics were collected at the MILES baseline visit by structured interview. We compared access between cases and frequency-matched controls (using chi-squared tests) and examined factors associated with access in separate multivariable logistic regression models.
Results: 654 participants (462 SLE cases, 192 controls) completed the MILES Cohort baseline visit; 584 (89.3%) female, 288 (44%) black, and mean age 53 years. SLE patients were significantly more likely than controls to report the following in the preceding 12 months to save money: skipping doses, taking less medicine, delaying filling prescriptions and asking their doctor for a lower cost medication (Table 1).
Table 1. Self-reported prescription access within the preceding 12 months in SLE cases compared to frequency-matched controls.
|
Questionnaire Item |
SLE cases (n=462) n (%) |
Controls (n=192) n (%) |
p-value |
|
Unable to get Rxs doctor felt necessary? |
56 (12.1) |
18 (9.4) |
NS |
|
Skipped med doses to save money? |
62 (13.4) |
12 (6.3) |
0.008 |
|
Taken less medicine to save money? |
70 (15.2) |
11 (5.7) |
0.001 |
|
Delayed filling a Rx to save money? |
75 (16.2) |
17 (8.9) |
0.013 |
|
Asked doctor for lower cost medication to save money? |
110 (23.8) |
30 (15.6) |
0.02 |
|
Bought Rx from another country to save money? |
5 (1.08) |
2 (1.04) |
NS |
|
Used alternative therapies to save money? |
38 (8.2) |
11 (5.7) |
NS |
NS=not significant
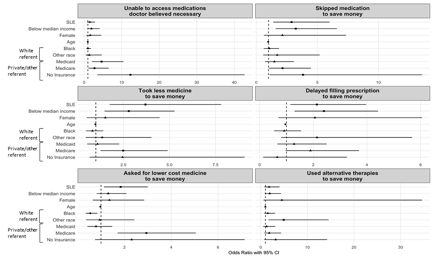
Based on multivariable models (Figure 1), having SLE was associated with several types of limitations in medication access, after adjusting for sex, race, age, insurance status, and income level. Household income below the US median was also associated with limitations in medication access, whereas private insurance was generally associated with improved access. Black persons were less likely to ask their doctor for lower cost alternatives.
Figure 1. Forest plots from a series of multivariable models of factors associated with aspects of prescription medication access and adherence. Squares represent positive odds ratios (ORs), circles negative ORs, triangles not significant ORs; horizontal lines represent 95% CIs.
Conclusion: SLE patients were more likely than controls from the general population to experience limitations in prescription medication access, and less than 1 in 4 patients asked providers for lower cost medications. Further, disparities in access were found in association with income, race and insurance status. Consideration of medication costs in patient decision making could provide a meaningful avenue for improving patient access and adherence to medications.
To cite this abstract in AMA style:
Minhas D, Marder W, Harlow S, Zick S, Hassett AL, Barbour KE, Helmick CG, Gordon C, Lee J, Padda A, McCune WJ, Somers EC. Patterns of Access to Prescription Medications Among Lupus Cases and Controls in the Population-Based Michigan Lupus Epidemiology & Surveillance (MILES) Cohort [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/patterns-of-access-to-prescription-medications-among-lupus-cases-and-controls-in-the-population-based-michigan-lupus-epidemiology-surveillance-miles-cohort/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patterns-of-access-to-prescription-medications-among-lupus-cases-and-controls-in-the-population-based-michigan-lupus-epidemiology-surveillance-miles-cohort/