Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: One-quarter to one-third of RA patients use long-term glucocorticoids (GCs) despite their known, dose-dependent association with increased risk of major adverse cardiovascular (CV) events (MACE). Little is known about patterns of GC use among RA patients with MACE risk factors (e.g. diabetes, smoking), or how GC use may potentiate these risk factors.
Methods: In this retrospective cohort study, we used administrative data to identify 6,090 RA patients with ≥1 visit to Veterans Health Administration rheumatology clinic during 2013-2017. We excluded patients with no disease-modifying anti-rheumatic drug use (n = 686) and confounding disorders also treated with GCs (n = 2,520). In the resulting 2,884-patient cohort, we used logistic regression to evaluate associations between incident MACE during 2013-2018 (outcome), recent long-term GC use (predictor), and baseline MACE risk factors (covariates). We included 5 MACE risk factors: hypertension, diabetes, hyperlipidemia, tobacco use, and prior MACE. To examine how GC use influences the effects of MACE risk factors, we included two-way interaction terms between GC use and each of the five MACE risk factors defined above.
We used a validated claims-based algorithm to define MACE as any of acute myocardial infarction, ischemic stroke, transient ischemic attack, sudden death, or coronary revascularization, occurring between index date and December 31, 2018. Index date was defined as the patient’s first rheumatology visit after meeting RA diagnostic criteria. We defined recent long-term GC use as ≥90 days’ supply dispensed during the two years preceding index date.
Results: Among 2,884 RA patients, 1,553 (54%) had MACE risk factors, and 97 (3%) had prior MACE (Table 1). Overall, 16% of patients recently used long-term GC, compared to 17% of patients with MACE risk factors, and 22% of patients with prior MACE. Incident MACE occurred in 308 (11%) patients, 24% of whom had recent long-term GC use. Recent long-term GC use was independently associated with increased incident MACE (Table 2). While no interaction term was statistically significant overall, differences in odds of incident MACE were seen across levels of recent GC use for several risk factors, particularly diabetes (OR 2.10, 95% CI [0.93-4.77]), tobacco use (OR 2.88, 95% CI [1.16-7.14]) and prior MACE (OR 2.41, 95% CI [0.73-7.95]) (Table 3).
Conclusion: Long-term GC use is common among RA patients with MACE risk factors, including those with prior MACE. In this cohort, a quarter of patients with an incident MACE had recently used long-term GC. Long-term GC use may potentiate the effect of comorbidities like diabetes and tobacco use, disproportionately increasing MACE risk in certain patients. Further work is needed to evaluate the effect of persistent long-term GC use after MACE events, and to explore how GC use may amplify the effects of other CV risk factors.
 Table 1: Baseline characteristics by risk of MACE, assessed at first VA rheumatologist visit during the study period.
Table 1: Baseline characteristics by risk of MACE, assessed at first VA rheumatologist visit during the study period.
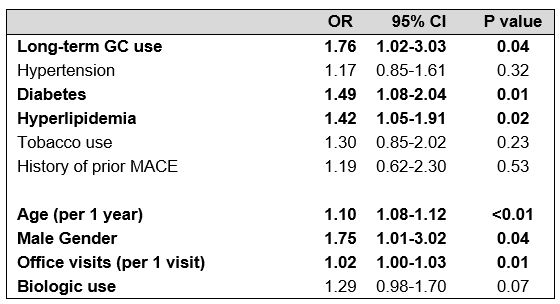 Table 2: Multivariable logistic regression model showing association between long-term GC use in the 2 years prior to index date and incident MACE.
Table 2: Multivariable logistic regression model showing association between long-term GC use in the 2 years prior to index date and incident MACE.
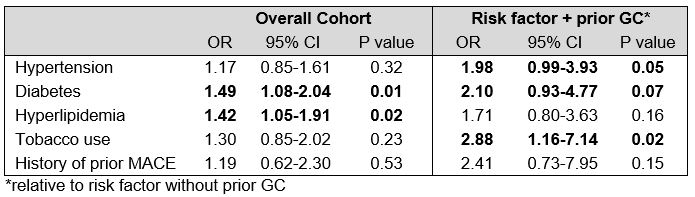 Table 3: Odds ratios for two-way interactions between long-term GC use and five MACE risk factors.
Table 3: Odds ratios for two-way interactions between long-term GC use and five MACE risk factors.
To cite this abstract in AMA style:
Wallace B, Gao Y, Roul P, England B, Mikuls T, Cohen-Mekelburg S, Clauw D, Hayward R, Waljee A. Patterns and Impact of Long-term Glucocorticoid Use on RA Patients at Risk for Major Adverse Cardiac Events [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/patterns-and-impact-of-long-term-glucocorticoid-use-on-ra-patients-at-risk-for-major-adverse-cardiac-events/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patterns-and-impact-of-long-term-glucocorticoid-use-on-ra-patients-at-risk-for-major-adverse-cardiac-events/
