Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Atlantoaxial joint involvement in calcium pyrophosphate deposition disease (CPPD) may present as crowned dens syndrome (CDS), a clinico-radiological tetrad defined as the presence of periodontoid calcifications, acute cervical pain with neck stiffness, fever, and raised inflammatory markers. Though 40-60% of CPPD patients exhibit periodontoid calcifications, only a small percentage develop CDS. Risk factors associated with CDS development in these patients remain unknown. The purpose of this study was to identify differences between symptomatic and asymptomatic CPPD patients with periodontoid calcifications.
Methods: Single-center cross-sectional analysis of CPPD patients with periodontoid calcifications identified by cervical or head CT done for various unrelated reasons. All the analyses were performed using STATA 14.2.
Results: Forty-one patients with CPPD and periodontoid calcifications were identified. Median age at diagnosis was 78 years (73-83) and 26 (63.4%) were female. Peripheral arthritis was present in 27 patients (65.9%) as monoarthritis (8), oligoarthritis (11), or polyarthritis (8). All patients had radiographic chondrocalcinosis at other sites. Metabolic changes were present in 20 patients (48.8%): low 25(OH)D (17), hyperparathyroidism (9), hypomagnesemia (2), and hypophosphatemia (1). Eleven patients had chronic kidney disease (26.8%). Periodontoid calcifications were documented at the transverse (cruciform) ligament in 39 patients (95.1%), alar ligaments in 19 (46.3%), and apical ligament in 6 (14.6%). CT staging of the transverse ligament changes identified curvilinear deposits ( >1mm) in a single band (stage 2) in 23 patients (56.1%).
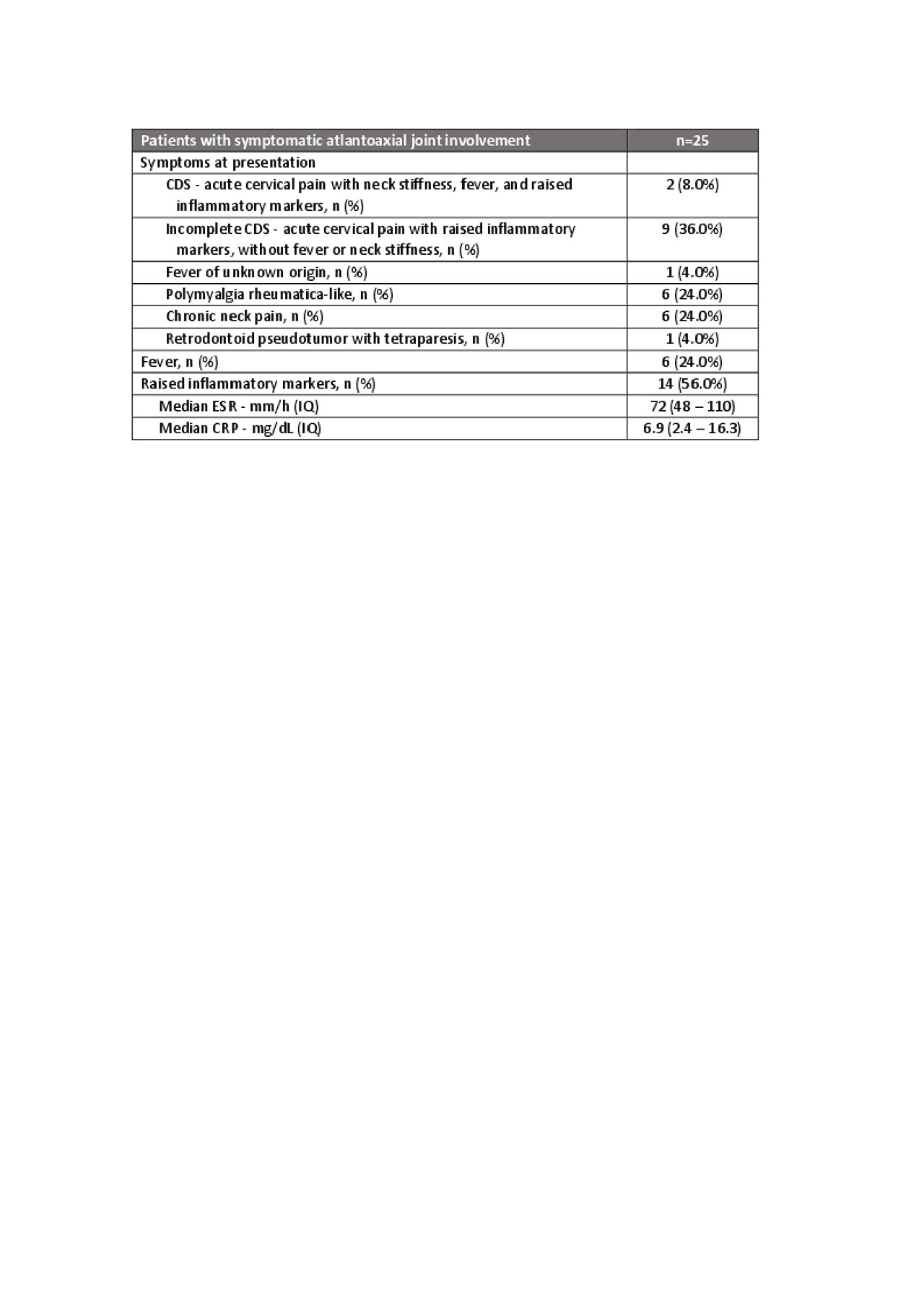
Twenty-five patients (61.0%) had symptomatic atlantoaxial joint involvement (Table 1). All symptomatic patients were treated with a combination of colchicine (16; 64.0%), NSAIDs (13; 52.0%), and/or systemic corticosteroids (13; 52.0%). Four patients (16.0%) with peripheral polyarthritis were treated with methotrexate.
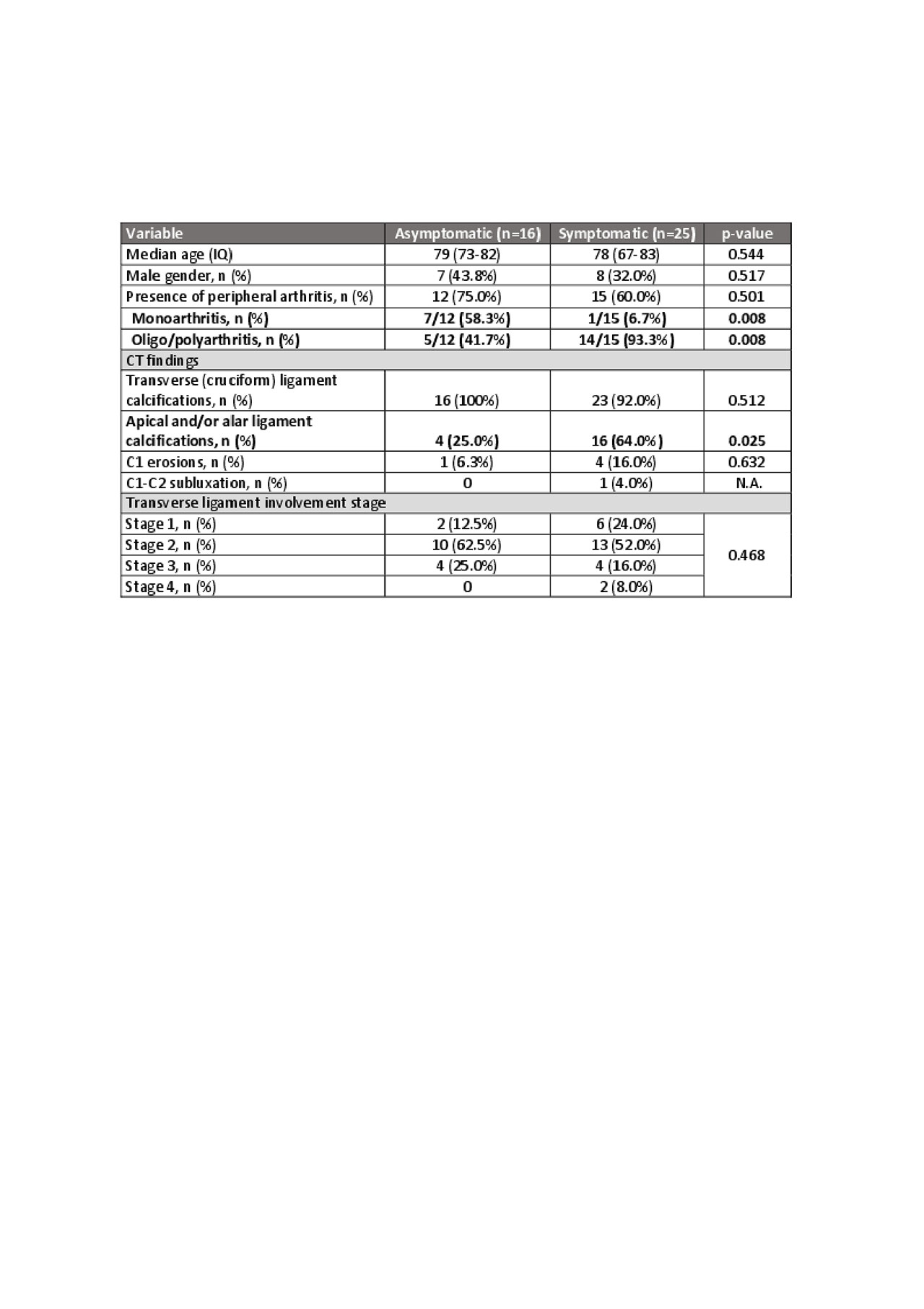
Comparative analysis (Table 2) showed that, in patients with peripheral arthritis, monoarthritis was more frequent in patients with asymptomatic periodontoid calcifications and oligo/polyarthritis was more common in patients with symptomatic disease. Apical and/or alar ligament calcifications were more frequent in patient with symptomatic atlantoaxial joint involvement.
Conclusion: Atlantoaxial joint involvement in CPPD is heterogeneous, classical CDS being uncommon. The pattern of peripheral arthritis and ligament calcification is associated with the presence of symptoms in CPPD patients with periodontoid calcifications.
To cite this abstract in AMA style:
Silva-Dinis J, Tenazinha C, Khmelinskii N, Teixeira V, Ávila-Ribeiro P, Eurico Fonseca J, Romeu J. Patterns and Clinico-Radiological Correlates of Symptomatic Atlantoaxial Joint Involvement in Patients with Calcium Pyrophosphate Deposition Disease [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/patterns-and-clinico-radiological-correlates-of-symptomatic-atlantoaxial-joint-involvement-in-patients-with-calcium-pyrophosphate-deposition-disease/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patterns-and-clinico-radiological-correlates-of-symptomatic-atlantoaxial-joint-involvement-in-patients-with-calcium-pyrophosphate-deposition-disease/