Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Osteoarthritis Management Programs (OAMPs) were developed to address gaps in provision of evidence-based treatments by offering individualized, comprehensive, non-operative care. Early data reveal improvements in patient pain and functioning, and enhanced scores for patient-reported quality-of-care indicators. But patient perceptions of this model are unclear. This qualitative study assessed patient feedback on an OAMP that offered team-based care in one-on-one or group medical visit settings.
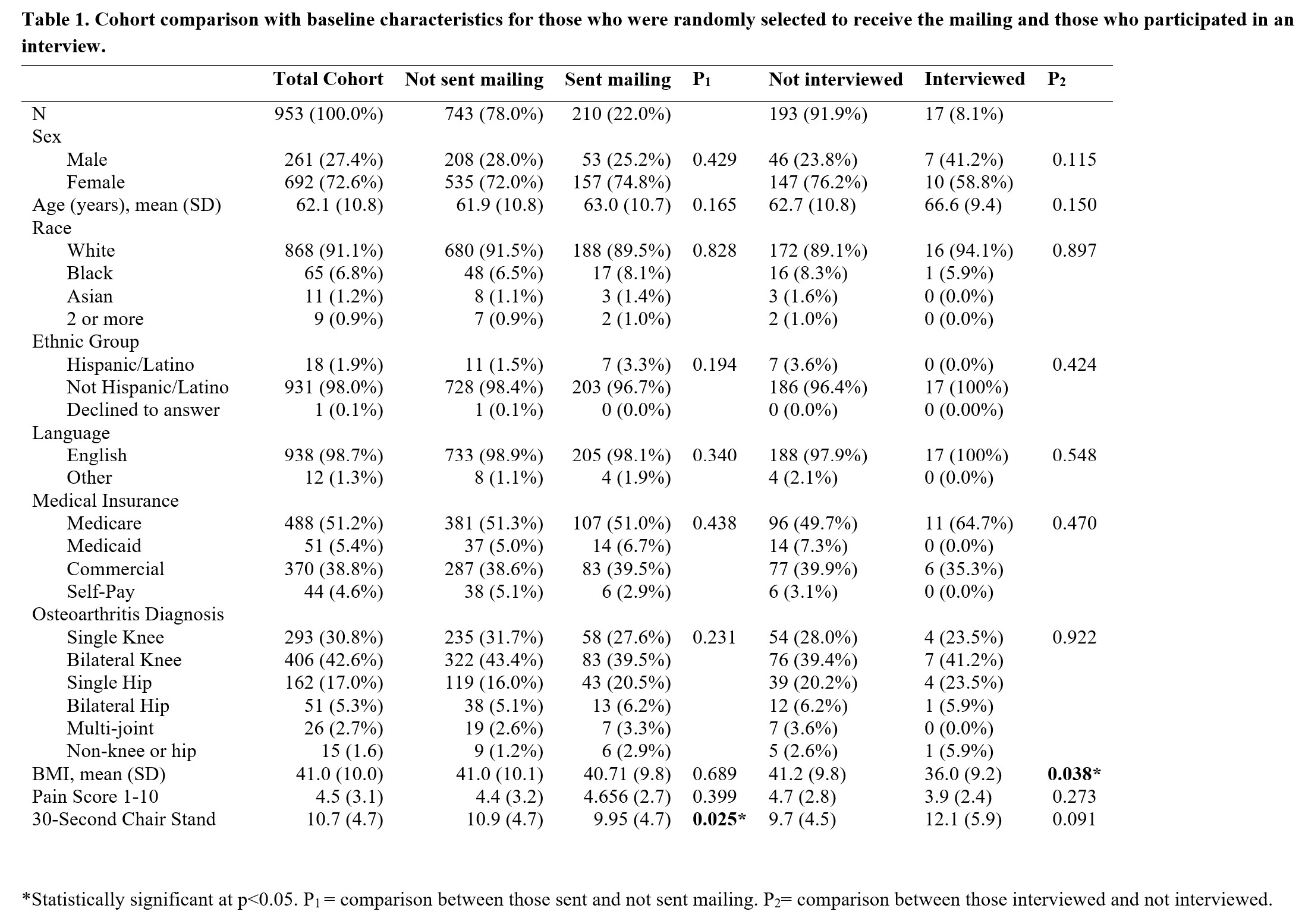
Methods: Adult patients who completed one or more OAMP visits from 7/1/2017-1/15/2021 were sorted into three groups based on number of visits: 1, 2-3, and 4+. Seventy patients from each group were sent a mailing with an invitation to participate in a 45-minute interview about their OAMP experiences. Interested patients were instructed to sign and return the study consent form, and to leave a telephone message indicating their desire to be interviewed. The voicemail box was checked daily and interviews were conducted until no additional data were found. Participants received $25 for completing the interview. Interviews were conducted in-person or via telephone by a trained interviewer who followed a semi-structured script. All interviews were audio recorded and transcribed verbatim. Three members of the investigative team analyzed the interviews manually. They independently performed line-by-line coding, utilizing software for data organization and retrieval to create categories of initial codes, then arriving at parent themes. Deductive and inductive thematic analyses identified daughter themes. Differences were discussed until consensus was reached for all coding progressions.
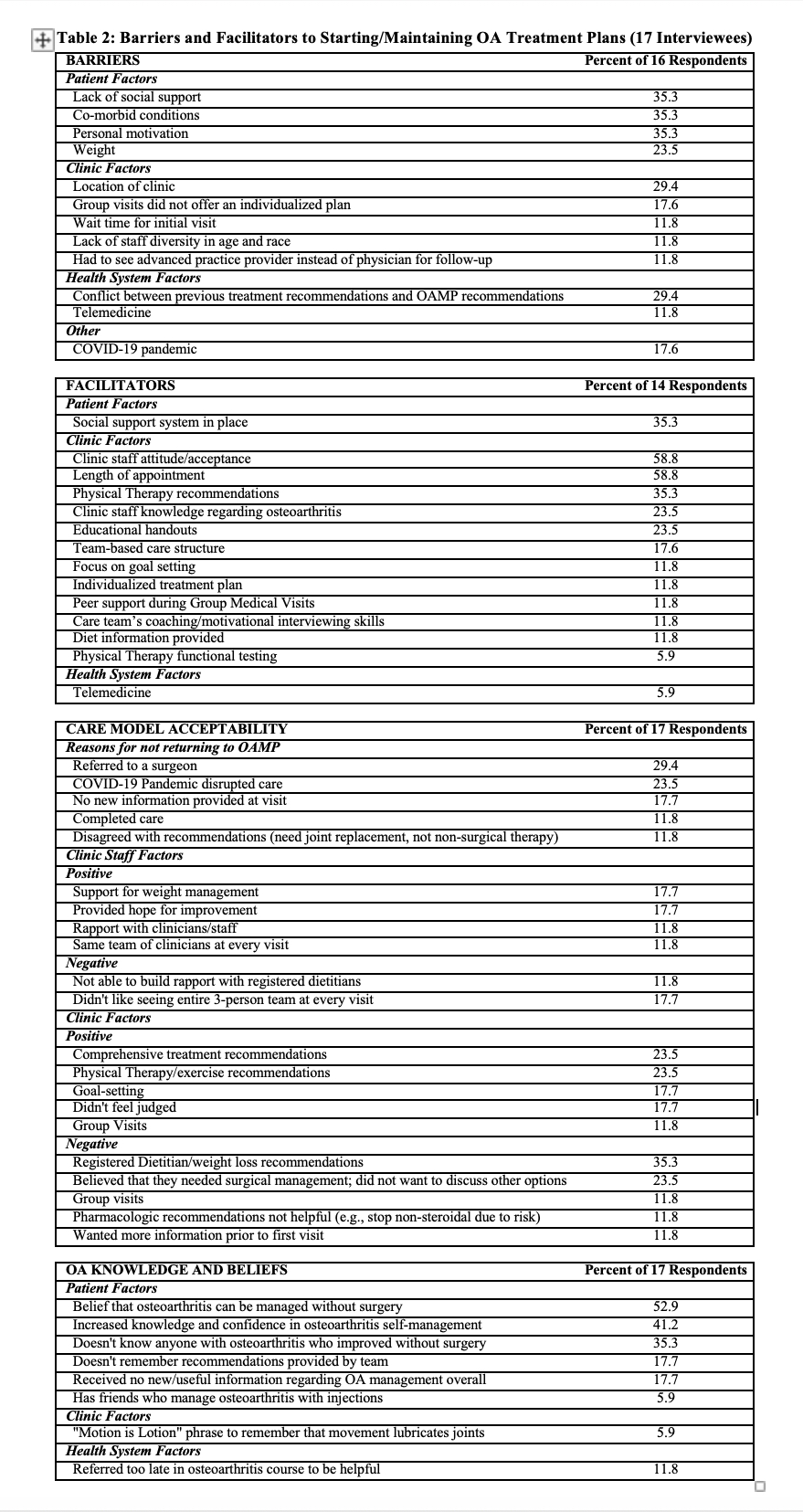
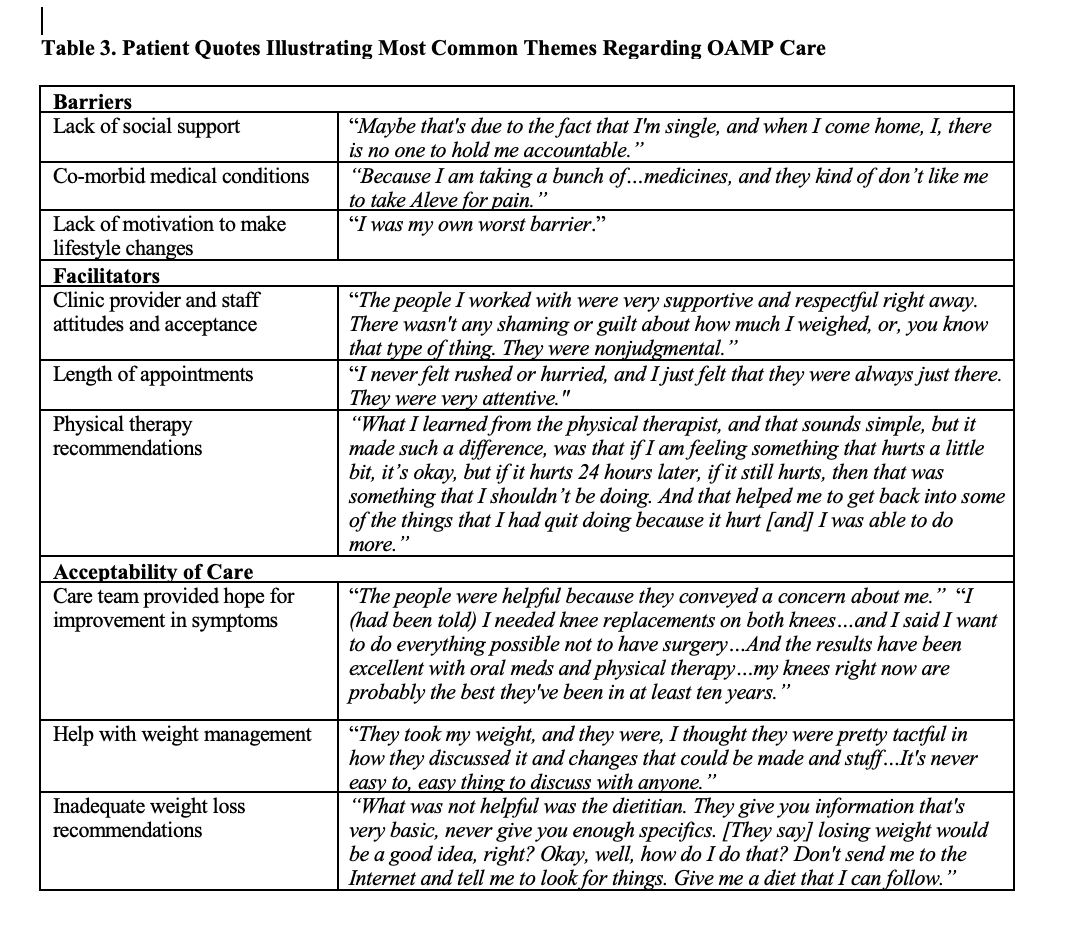
Results: A total of 953 eligible patients were identified. The 210 randomly selected to be sent the mailing were similar in characteristics to the 743 who were not sent the mailing. Data saturation was reached at 17 interviews. Interviewees were similar in characteristics to the 193 who did not interview, except for body mass index (36.0 and 41.2 respectively, p=0.038). Sixteen (94.1%) patients identified at least one barrier to starting and/or maintaining their osteoarthritis treatment plans. The most common barriers were a lack of social support (35.3%), co-morbid medical conditions (35.3%), and a lack of motivation to make lifestyle changes (35.3%). Fifty-three percent of interviewees endorsed the belief that osteoarthritis can be managed without surgery and 41.2% reported increased knowledge and confidence in self-management.
Conclusion: OAMPs were designed to bridge gaps in recommended and received care. Our patients reported improvements in knowledge and attitudes regarding non-surgical treatment, but identified barriers that warrant adjustments to delivery of care. This feedback may be useful for other health care systems who have, or are considering implementation of, an OAMP.
To cite this abstract in AMA style:
Lasinski A, Miller K, Robniak A, Morgan A, Baier Manwell L. Patient Perceptions of an Osteoarthritis Management Program at a Midwest Medical Center [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/patient-perceptions-of-an-osteoarthritis-management-program-at-a-midwest-medical-center/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-perceptions-of-an-osteoarthritis-management-program-at-a-midwest-medical-center/