Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Repeat hospitalizations in patients with pulmonary hypertension from all causes are associated with worse survival. However, predictors of systemic sclerosis associated pulmonary hypertension (SSc-PH) readmissions are unknown. The objective of this study is to identify patient-level factors associated with readmission among SSc-PH patients.
Methods: This retrospective study used clinical data from the prospective observational Pulmonary Hypertension Assessment and Recognition of Outcomes in Scleroderma (PHAROS) registry. All patients met the 2013 ACR/EULAR classification criteria for SSc. PH was defined as a mean pulmonary artery pressure ≥25 mmHg on right heart catheterization. The PHAROS investigators collected data for each hospitalization’s primary reason and admission date. Readmission was defined as a subsequent hospitalization for any reason within 12 months. We compared patient-level characteristics of individuals with vs. without readmission using Fisher’s exact test and the Wilcoxon rank-sum test. Logistic regression models were used to estimate associations between clinical variables and likelihood of readmission. Odds ratios (OR) and 95% confidence intervals (CI) were calculated for all estimates. Survival comparisons were made using the log-rank test.
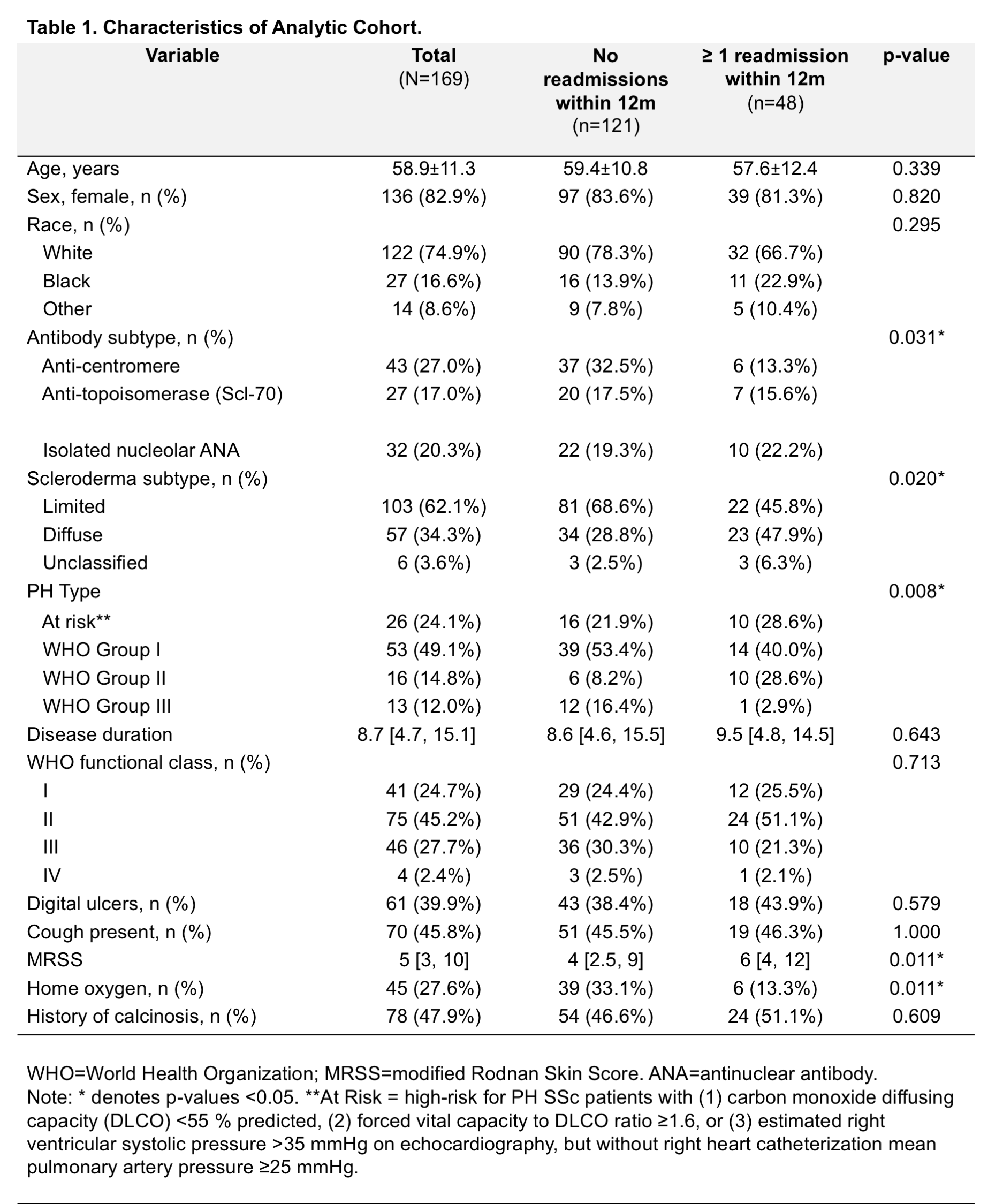
Results: Of 335 SSc-PH patients, 169 (50%) had at least 1 hospitalization. Of these, 48 (28%) had a readmission. Patients with vs. without readmission more commonly had diffuse disease (p=0.02), positive Scl-70 autoantibody status (p=0.03), World Health Organization (WHO) Group 2 PH (p=0.01), higher modified Rodnan Skin Score (p=0.01), and did not require home oxygen (p=0.01) (Table 1). Patients with diffuse vs. limited disease were significantly more likely to have a readmission (OR 2.49; 95% CI 1.23-5.06). Readmission was less likely in individuals who required vs. did not require home supplemental oxygen (OR 0.28; 95% CI 0.09-0.88) and in those with vs. without desaturation during a 6 minute walk test (0.11; 95% CI 0.01-0.90). Fifty-four patients died. Mortality rates were higher in patients with ≥2 vs. 0-1 readmission (66% vs. 30.6%, p=0.009) and similar in patients with 0 vs. 1 readmission (30.6% vs. 31%, p=0.561). Race, age, sex, SSc disease duration, and patient reported outcomes were not significantly associated with readmission.
Conclusion: Readmission was more common among SSc-PH patients with diffuse disease, WHO Group 2 PH, and positive Scl-70 autoantibody status. These patients may benefit from closer post-hospitalization follow-up. Home oxygen use was associated with lower likelihood of readmission and can be routinely assessed at the time of discharge in SSc-PH patients. Future studies should determine if universal testing for the need for home supplemental oxygen at the time of discharge reduces readmission among SSc-PH patients.
To cite this abstract in AMA style:
Showalter K, Pinheiro L, Szymonifka J, Sobol I, Steen VD, Gordon JK. Patient-Level Factors Associated with Hospital Readmission Among Patients with Systemic Sclerosis Associated Pulmonary Hypertension [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/patient-level-factors-associated-with-hospital-readmission-among-patients-with-systemic-sclerosis-associated-pulmonary-hypertension/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-level-factors-associated-with-hospital-readmission-among-patients-with-systemic-sclerosis-associated-pulmonary-hypertension/