Session Information
Date: Sunday, November 12, 2023
Title: (0252–0282) Miscellaneous Rheumatic & Inflammatory Diseases Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Noninfectious inflammatory eye disease (NIIED) is a sight-threatening condition with two-thirds of patients incurring prolonged vision loss due to uncontrolled ocular inflammation. Non-glucocorticoid systemic therapy (NGST) effectively induces and maintains remission in NIIED. However, minimal research exists on the risk factors for requiring long-term NGST for NIIED control or for NIIED relapse after discontinuation of NGST.
Methods: We performed a retrospective chart review of NIIED patients who were evaluated by the Cleveland Clinic Ophthalmology and Rheumatology departments and initiated NGST between January 1, 2014 through December 31, 2018, and had at least 4 years of follow-up prior to December 31, 2022. If treatment was dictated by systemic disease, patients were excluded. Data were extracted from the electronic medical record. The association between patient characteristics and the groups were analyzed through univariate logistic regression.
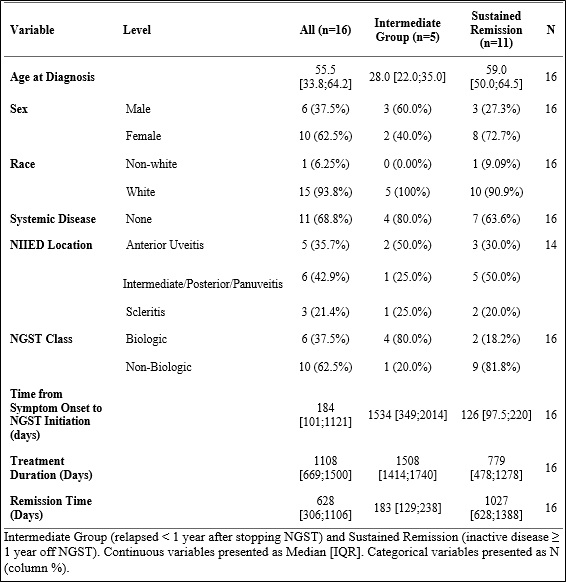
Results: 94 NIIED patients were included in the study. 78 patients (83.0%) were maintained on NGST throughout the study period, designated as long-term NGST. 16 patients (17.0%) had NGST discontinued due to inactive NIIED, denoted as short-term NGST. NIIED location was significantly different between the two groups (Table 1). Patients with intermediate, posterior, or pan uveitis were more likely to require long-term NGST compared to patients with anterior uveitis (Table 2). Age, sex, race, presence of systemic disease, and treatment with biologic or nonbiologic medication were not significantly different between the groups. However, data trends showed that patients with white race were more likely to require long-term NGST than non-white race; earlier initiation of NGST was more represented in the short-term NGST group which may imply that earlier initiation of NGST confers a greater likelihood of discontinuing NGST due to inactive NIIED. Within the short-term NGST group, 11 patients (68.8%) had inactive NIIED for ≥ 1 year, designated as sustained remission, and 5 patients (31.3%) had relapse of active NIIED < 1 year, designated as intermediate group. NIIED patients with sustained remission tended to be diagnosed at an older age and had earlier initiation of NGST than the intermediate group (Table 3).
Conclusion: This study provides insight into the risk factors for requiring long-term NGST and sustained remission for patients with NIIED. Our results demonstrate that NIIED location of intermediate, posterior, or pan uveitis is a risk factor for requiring long-term NGST. Older age and earlier initiation NGST may be associated with sustained remission of NIIED.
To cite this abstract in AMA style:
Koenig T, Fell D, Mammo D, Zhang C, Srivastava S, Lowder C, Sharma S, Hajj-Ali R. Patient, Disease, and Treatment Factors in Remission of Inflammatory Eye Disease [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/patient-disease-and-treatment-factors-in-remission-of-inflammatory-eye-disease/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-disease-and-treatment-factors-in-remission-of-inflammatory-eye-disease/