Session Information
Date: Monday, November 18, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Compared with the general population, patients with psoriatic arthritis (PsA) have a higher risk of comorbidities and all-cause mortality. They are also at increased risk of complications of treatment (e.g., opportunistic infections) and existing comorbidities (e.g., myocardial infarction related to cardiovascular disease), that could prompt an emergency department (ED) visit. Reasons patients with PsA present to the ED and resultant outcomes have not been studied. We, therefore, evaluated the patient characteristics and outcomes associated with ED visits in patients diagnosed with PsA using the largest all-payer ED database in the U.S., the Nationwide Emergency Department Sample (NEDS).
Methods: We used NEDS (2019) to identify ED visits for adults aged ≥18 years with a PsA diagnosis based on the presence of ≥1 International Classification of Diseases (ICD) codes L40.5x. We compared baseline demographics (age, sex, race/ethnicity, primary insurance payer, and income quartile) and clinical comorbidities linked to ED visits with PsA, compared to those without the above codes for PsA. We assessed the top three primary diagnoses associated with inpatient admission among PsA ED visits. Pearson chi squared tests were used to compare categorical variables and t-tests to compare continuous variables among groups. We performed multivariable logistic regression, accounting for age, sex, race/ethnicity, income, and clinical comorbidities to calculate odds ratios (ORs) and 95% confidence intervals (CIs) of association of different factors to inpatient admission in PsA ED visits.
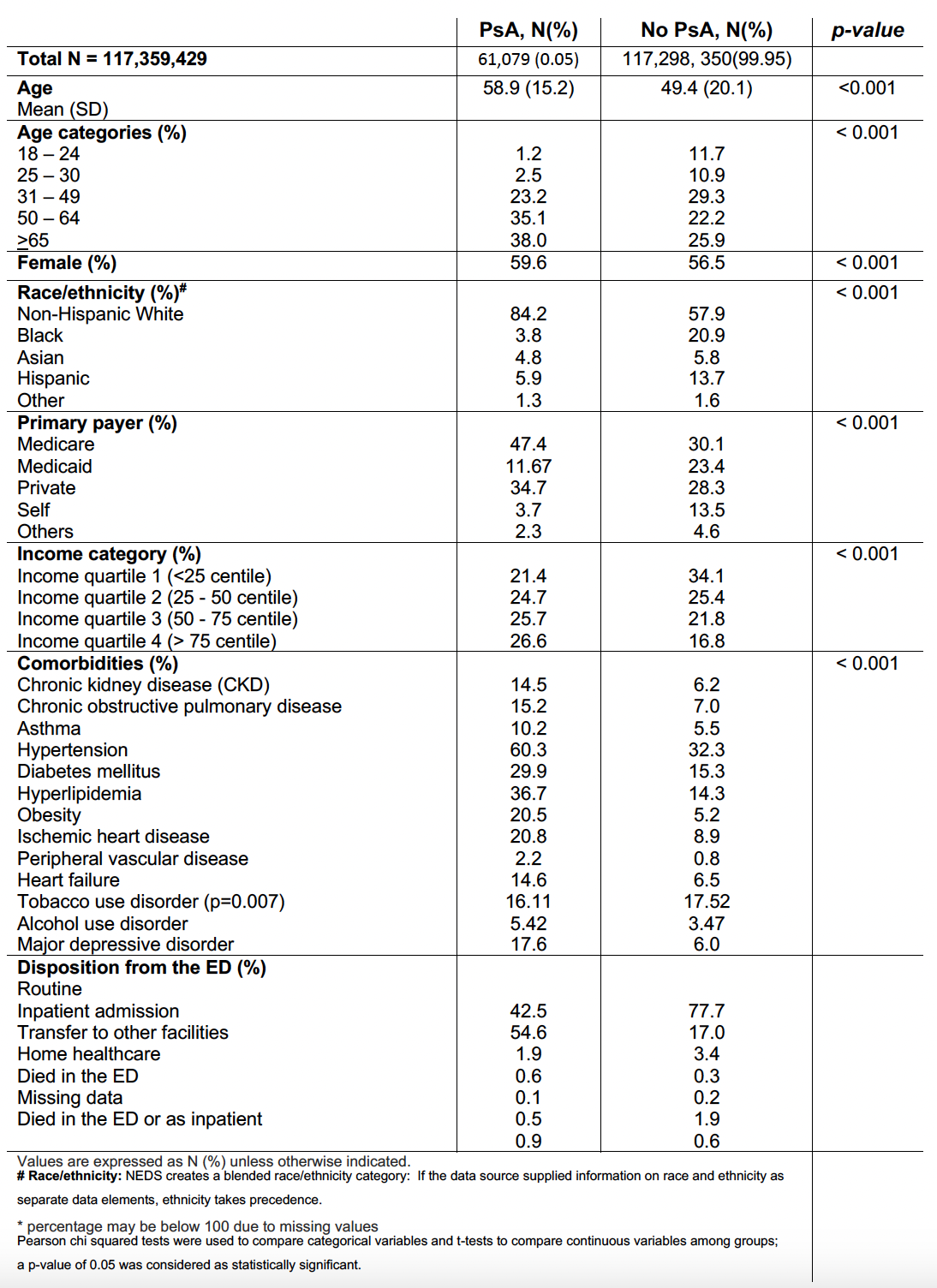
Results: Of a total of 117,359,429 ED visits for adults ages >18 years, 61,079 (0.05%) ED visits had a PsA diagnosis (mean age 59 ±15.2 years, 59.6% female, 84% non-Hispanic White, 47.4% with Medicare as primary insurance) (Table 1). Among ED visits without PsA, the mean (SD) age was 49.4 years (20.1), 56.5% were female, 58% were non-Hispanic White and 30.1% had Medicare as their primary insurance. Of the PsA ED visits, 55% resulted in admission compared to 17% in those without PsA. The three most common diagnoses associated with hospital admission in PsA patients were septicemia, skin and subcutaneous tissue infections, and heart failure.
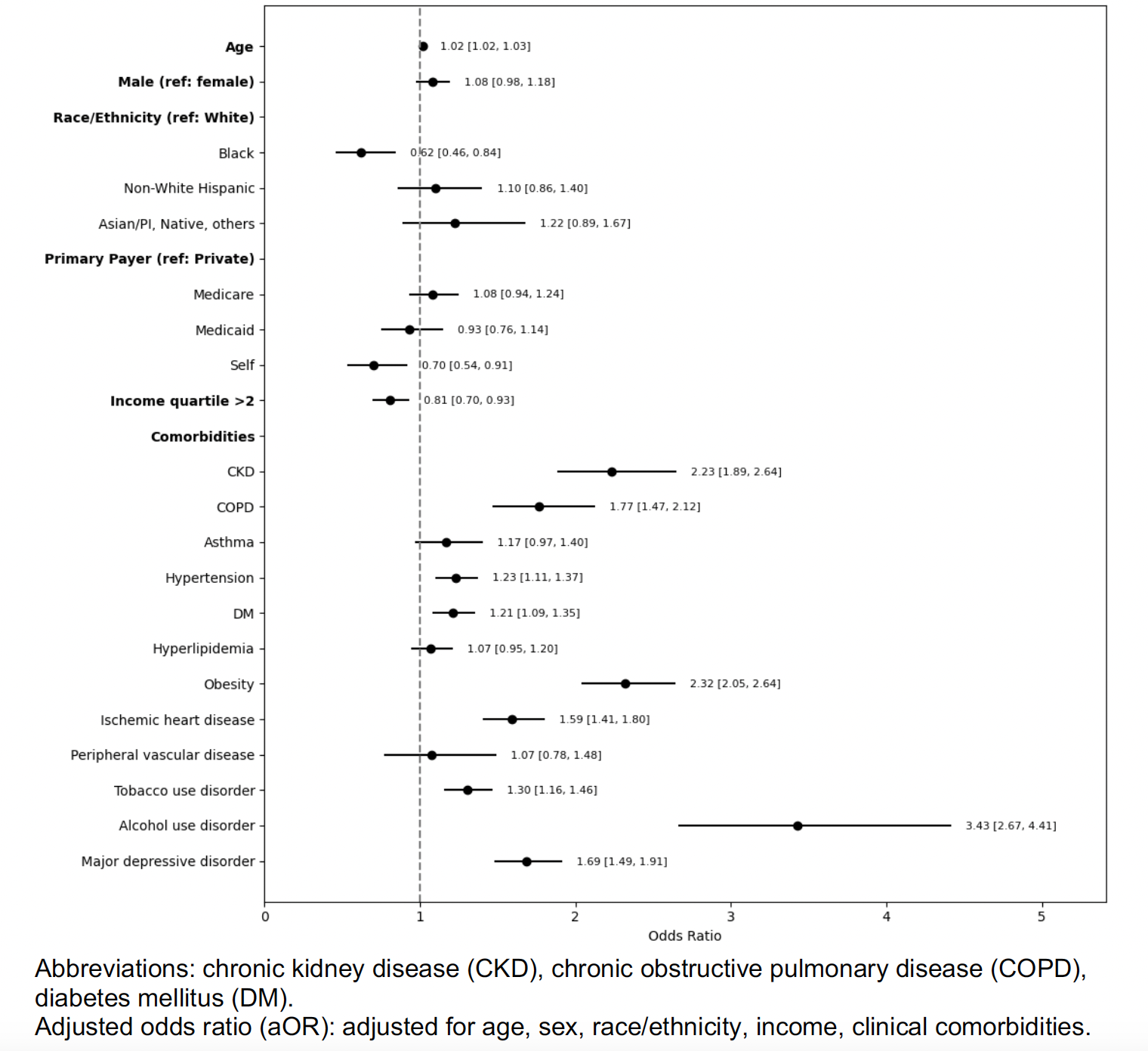
In multivariable analyses, some factors associated with increased odds of inpatient admission among PsA ED visits included older age (OR 1.02, 95% 1.018-1.03), stroke (OR 4.83, 95% CI 3.02 – 7.72), alcohol use disorders (OR 3.43, 95% 2.66-4.41), obesity (OR 2.32, CI 2.05-2.64), chronic kidney disease (OR 2.23, 95% CI 1.80-2.64) (Figure 1). Black race (OR 0.62, CI 0.46-0.84) and median income < 50th quartile (OR 0.80, CI 0.70-0.92) were associated with a lower odds of admission compared to non-Hispanic White patients.
Conclusion: In this large U.S. sample of adults presenting to the ED, those with PsA tended to be older, of female sex, non-Hispanic White, and primarily insured by Medicare compared to those without PsA. Over half of ED PsA patients were admitted. Future work should focus on PsA domains involved, medications, and lab values that predict ED visits, while also focusing on reducing health disparities in vulnerable populations.
To cite this abstract in AMA style:
Feterman Jimenez D, Stovall R, Porres Arnaez J, Bharadiya V, Liew J, Bays A, Jenna T, Robinson L, Dhital R, Singh N. Patient Characteristics and Outcomes of Emergency Visits in Psoriatic Arthritis: Results from the U.S. Nationwide Emergency Department Sample (NEDS) [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/patient-characteristics-and-outcomes-of-emergency-visits-in-psoriatic-arthritis-results-from-the-u-s-nationwide-emergency-department-sample-neds/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-characteristics-and-outcomes-of-emergency-visits-in-psoriatic-arthritis-results-from-the-u-s-nationwide-emergency-department-sample-neds/