Session Information
Date: Sunday, November 10, 2019
Title: Education Poster
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Palliative care is a specialty that focuses on holistic care, promoting quality of life, and providing an extra layer of support for patients and families alongside traditional medical treatment. While these principles are highly relevant to many patients seen by rheumatologists, palliative care education for rheumatologists has been limited. Our aim was to assess the baseline needs of rheumatologists in our division, present an educational program, and identify opportunities for adaptation and expansion of palliative care education.
Methods: We developed an educational program collaboratively with palliative care that was presented to Rheumatology faculty and fellows at the University of Pennsylvania in the fall of 2018. A needs assessment survey was developed based on well-known palliative care concepts to assess baseline skills and attitudes. A two-hour interactive session was held based on the established and validated “Serious Illness Care Program” created by Ariadne Labs, adapting content to rheumatology. This program includes teaching the “Serious Illness Conversation Guide” – a scripted set of questions to guide clinicians through a conversation that includes 1) setting up the conversation, 2) assessing patient understanding, 3) sharing information, 4) exploring patient goals, fears, strengths, wishes, and 5) closing. The session included a demonstration of how to utilize the Conversation Guide, break-out sessions to practice conversations led by palliative care specialists using rheumatology-specific cases, and a debrief. Two champions of the program were identified who trialed the guide in clinic over the following four months. All providers received a follow-up survey to evaluate the program.
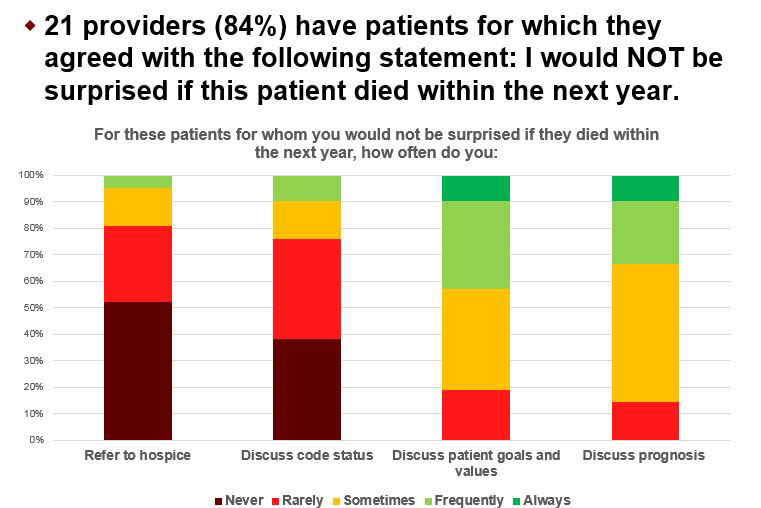
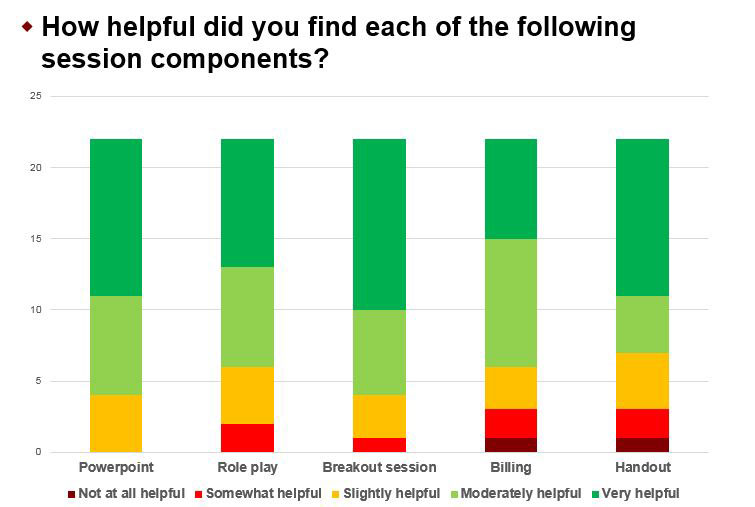
Results: The needs assessment survey had 25/30 responses. No providers had received previous rheumatology-specific palliative care training and 36% had never received any palliative care training. 21 (84%) reported seeing patients for which they would not be surprised if the patient died within the next year. Few providers referred to hospice or discussed code status, and a minority regularly discussed patient goals/values or prognosis for these patients (Figure 1). Time and uncertainty in prognostication were the most significant barriers to these conversations. The two-hour session was attended by 27 providers. In the follow-up survey, >80% found the program to be interesting, appropriate in length, and appropriate in scope. Each component of the program was favorably rated (Figure 2). Although only two providers were designated as “champions,” 6 providers reported using the Conversation Guide in clinic. Time was the major barrier to using the guide.
Conclusion: This innovation was among the first to adapt a validated palliative care training program to a rheumatology division. The program was highly rated and led to use of the Conversation Guide in clinic. Further adaption of the Conversation Guide to rheumatology specific needs, scheduling changes to allow time for serious illness conversations in clinic, and assessment of benefits to patients are planned.
To cite this abstract in AMA style:
Karpoff M, George M, Dingfield L. Palliative Care Curriculum in Rheumatology: Teaching Serious Illness Conversations [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/palliative-care-curriculum-in-rheumatology-teaching-serious-illness-conversations/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/palliative-care-curriculum-in-rheumatology-teaching-serious-illness-conversations/