Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Cataract is one of the most common and visually debilitating complications of paediatric uveitis developing as a consequence of chronic inflammation and steroid use. Cataract surgery can be technically challenging in patients with uveitis and the outcomes less certain.(1) Inserting an intraocular lens (IOL) is controversial for paediatric uveitis patients leading to variable practice across different institutions. This study compares the outcomes of cataract surgery associated with paediatric uveitis with or without IOL implantation.
Methods: A retrospective comparison study was conducted at two centres, Bristol Eye Hospital (Centre 1-Cataract surgery with IOL implantation) and Sheffield Children’s Hospital (Centre 2-Cataract surgery without IOL implantation). All children below 18 years of age with uveitis who underwent cataract surgery between year 2011 and 2024 were included. Pre and post operative outcomes from the two groups were compared, including best corrected visual acuity(BCVA), LogMAR lines of improvement, ocular inflammation and complications. Follow up data upto 2 years post-surgery where available were recorded. Data was analysed using descriptive statistics.
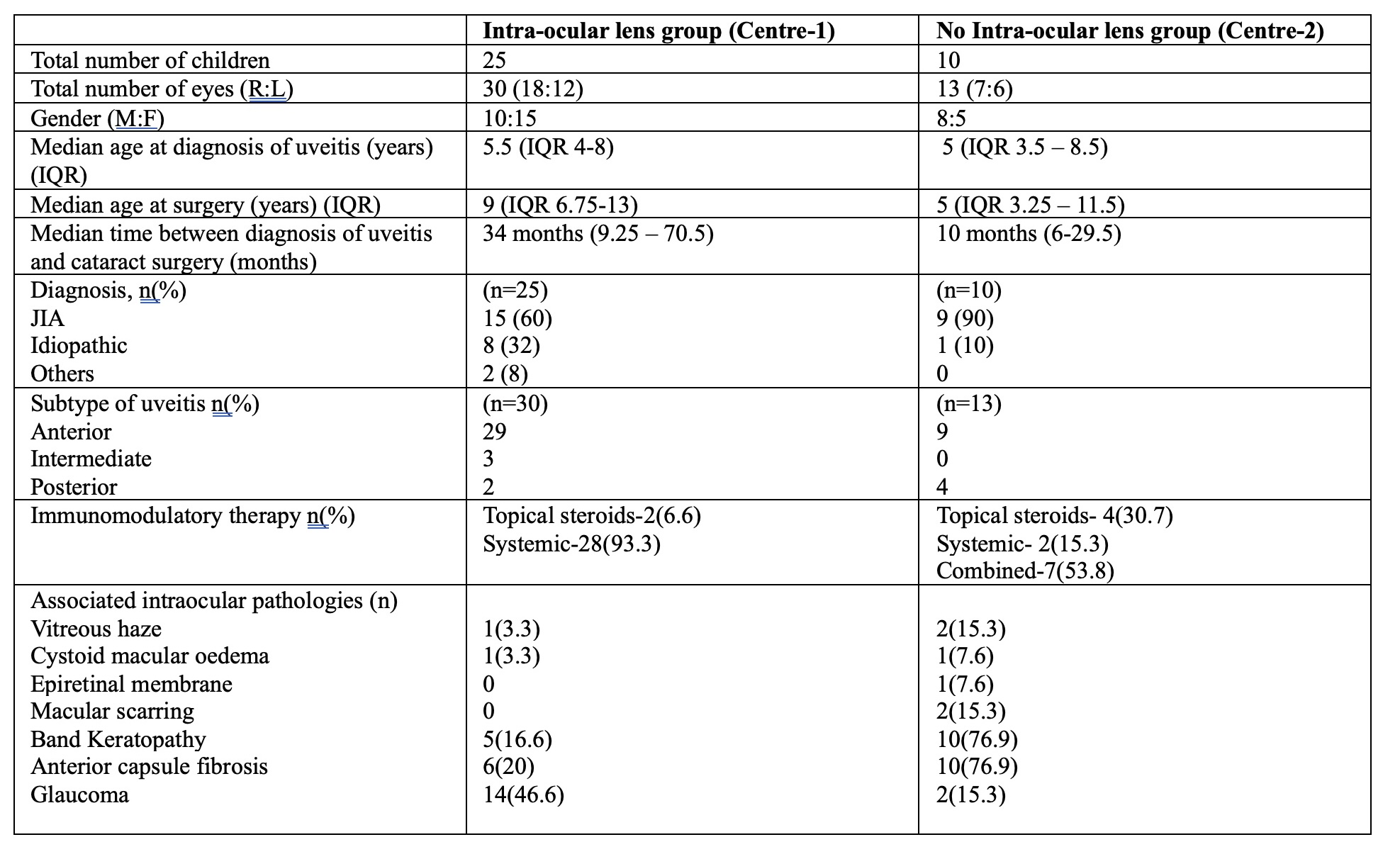
Results: There were total 35 children (43 eyes) identified from both centres, 25 children (30 eyes) from centre-1 and 10 children (13 eyes) from centre 2. The median age at diagnosis in years was 5.5years(centre 1) and 5years (centre 2) and median age at surgery was 9 and 5 years with M:F=2:3 and 1.6:1 respectively. JIA was the most common etiology at both centres (60% and 90% respectively). Anterior uveitis was the most common subtype of uveitis at both centres (29 eyes, 9 eyes respectively)-Table1. Surgical capsulotomy was required in 3 eyes (10%) by 24 months at centre 1. Active anterior chamber inflammation >1+ cells was recorded in 10(33%), 8(36.4%), 5(16.7%) in centre-1 and 1(7.7%), 2(15.4%), 1(7.7%) in centre-2 at 3,12 and 24 months.(Table2) Median preoperative BCVA (IQR) was 0.84 (0.60-1.43) and 1.6 (0.92- 2.48) respectively. The median post-operative BCVA at 3 months, 12 months and 24 months at centre 1 was 0.20,0.2 and 0.10 and at centre 2 was 0.38, 0.50 and 0.15. Percentage of children with 2 or more lines of improvement at 3,12 and 24 months at centre 1 was 82.8%, 93.1% and 80.8% whereas at centre 2 was 84.6%, 75% and 81.8%.(Table3)
Conclusion: Good visual improvement following cataract surgery in children with uveitis with and without IOL would support either of the practices. However, a caveat being that IOL insertion could potentially be associated with active inflammation. References:1. Quiñones K, Cervantes-Castañeda RA, Hynes AY, Daoud YJ, Foster CS. Outcomes of cataract surgery in children with chronic uveitis. J Cataract Refract Surg. 2009 Apr;35(4):725–31.
Table:1 Demographic and Clinical comparison of the study groups
.jpg) Table-2: Grading of anterior chamber inflammation in eyes with and without IOL
Table-2: Grading of anterior chamber inflammation in eyes with and without IOL
.jpg) Table-3 Comparison of pre- and post-operative best corrected visual acuity and lines of improvement at 3, 12 and 24 months.
Table-3 Comparison of pre- and post-operative best corrected visual acuity and lines of improvement at 3, 12 and 24 months.
To cite this abstract in AMA style:
Govardhan C, Batchu Prithvi A, Aladaileh B, Cattermole E, Abdelsattar F, Guly C, Choi J, Keller J, V Ramanan A. Paediatric uveitis – Retrospective comparison of cataract surgery outcomes with or without intraocular lens implantation from two tertiary centres in United Kingdom [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/paediatric-uveitis-retrospective-comparison-of-cataract-surgery-outcomes-with-or-without-intraocular-lens-implantation-from-two-tertiary-centres-in-united-kingdom/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/paediatric-uveitis-retrospective-comparison-of-cataract-surgery-outcomes-with-or-without-intraocular-lens-implantation-from-two-tertiary-centres-in-united-kingdom/