Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: RAPID3 scores correlate well with disease-specific indices, including the Clinical Disease Activity Index (CDAI) in RA and Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) in axSpA, and are being widely used in clinical practice1,2. However, being a patient-reported outcome, RAPID3 can be affected by additional sources of pain, including fibromyalgia, prior joint damage, and psychosocial reasons such as anxiety or depression. Adding a physician global estimate (MD Glob) to RAPID3 (we termed it P4 index: pain, physical function, patient global, and physician (MD) global) may add an objective component and help filter out extraneous factors affecting disease activity measurements. In this observational study, we assessed performance of P4 index by comparing it against RAPID3 and CDAI in RA and RAPID3 and BASDAI in axSpA patients.
Methods: Consecutive patients with RA and axSpA under the care of three clinicians at one academic Rheumatology center completed the Multidimensional Health Assessment Questionnaire (MDHAQ) during their clinic visits with RAPID3 scores subsequently calculated. CDAI and BASDAI scores, respectively, were also recorded at the same visit and the clinician would separately report a physician global estimate (MD Glob) in the Electronic Medical Record. P4 score was calculated by adding MD Glob to the RAPID3 score (score range 0 to 40). Statistical significance between all scores was analyzed using Spearman correlation coefficients. Subgroup analysis was performed including only RA and axSpA patients with concomitant osteoarthritis, fibromyalgia, or anxiety/depression.
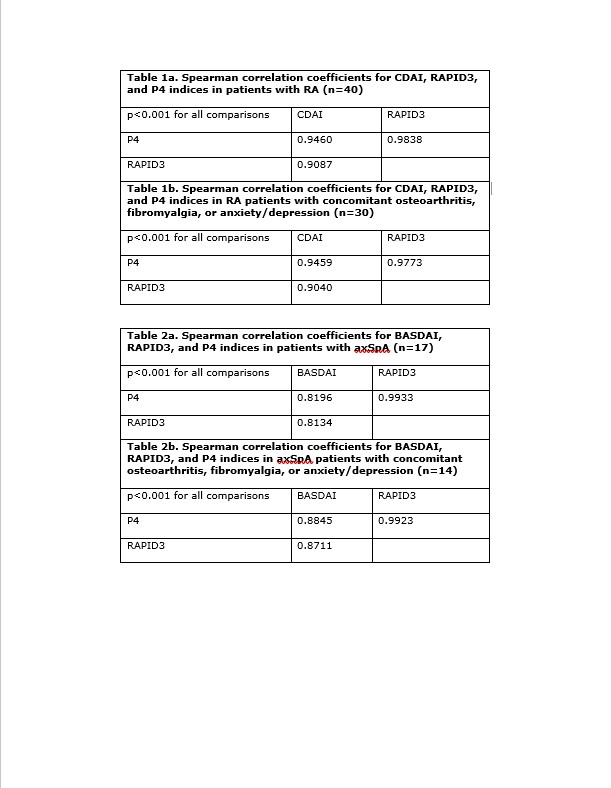
Results: We enrolled 40 patients with RA and 17 patients with axSpA; additional enrollment was limited by the coronavirus pandemic. Among RA patients, the mean (SD) CDAI was 8.8 (10.1), mean (SD) RAPID3 was 8.48 (7.9), and mean (SD) P4 was 11.2 (9.7). CDAI and RAPID3 correlated significantly (rho=0.91, p< 0.001). CDAI and P4 also correlated significantly and at somewhat higher levels than RAPID3 (rho=0.95, p< 0.001). Similar results were noted in subgroup analysis for RA patients (Table 1). Among axSpA patients, the mean (SD) BASDAI was 4.6 (2.5), mean (SD) RAPID3 was 12.7 (8.1), and mean P4 was 16.7 (9.9). BASDAI and RAPID3 correlated significantly (rho=0.81, p< 0.001). BASDAI and P4 also correlated significantly at a similar level (rho=0.82, p< 0.001). Subgroup analysis of axSpA patients showed similar results (rho=0.87 vs 0.88, see Table 2).
Conclusion: Our study demonstrates a high degree of correlation between P4 index and RAPID3 as well as validated disease-specific activity indices in both RA and axSpA patients. P4 index has an objective component in the form of MD Glob that may help to adjust for extraneous factors affecting disease activity measurement and management decisions. It would be important to confirm our findings in subsequent larger studies. Overall, using the P4 index may be a quick and practical way to more reliably trend disease activity in RA and axSpA.
1. Pincus T, et al. (2010) Arthritis Care & Research, 62(2):181-189.
2. Danve A, et al. (2015) J Clinical Rheumatology, 34:117-124.
To cite this abstract in AMA style:
Danve A, Hsiao B, Zhang P. P4 Index Correlates with RAPID3 and Disease-Specific Indices in Rheumatoid Arthritis (RA) and Axial Spondyloarthritis (axSpA) [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/p4-index-correlates-with-rapid3-and-disease-specific-indices-in-rheumatoid-arthritis-ra-and-axial-spondyloarthritis-axspa/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/p4-index-correlates-with-rapid3-and-disease-specific-indices-in-rheumatoid-arthritis-ra-and-axial-spondyloarthritis-axspa/