Session Information
Date: Sunday, November 13, 2022
Title: Abstracts: SLE – Diagnosis, Manifestations, and Outcomes II: Complications
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: To assess the prevalence of severe COVID-19 (COVID) overall and following vaccination among patients with systemic lupus erythematosus (SLE) and the general population, and within clinical subgroups.
Methods: Healthcare claims in the IBM® MarketScan® Commercial Database were used to identify adults (18+) with a confirmed SLE diagnosis between 1/1/2013 and 4/1/2020. The general population included all adults enrolled on 4/1/2020. Observation began 4/1/2020 and ended with the earliest of enrollment end, death, or 12/31/2021. COVID vaccination was identified by medical claims for vaccine administration or pharmacy claims for a vaccine. Prevalence was assessed for any COVID diagnosis (≥1 inpatient [IP] or outpatient [OP] claim with ICD-10 code U071 or J1282), IP COVID (≥1 IP COVID claim; “severe COVID”), COVID intensive care unit (ICU) admission (IP COVID with an ICU service or revenue code), COVID intubation (IP COVID with an intubation diagnosis or procedure code), and COVID death. Overall prevalence was assessed throughout the observation period; post-vaccination prevalence was defined as any COVID infection at least 14 days after first observed vaccination date. Demographics were assessed on 4/1/2020. Elixhauser Comorbidity Index (ECI) diagnoses were assessed among patients continuously enrolled in the 12 months before 4/1/2020. Unadjusted comparisons between SLE patients and the general population were made with chi-square and Fisher’s exact tests.
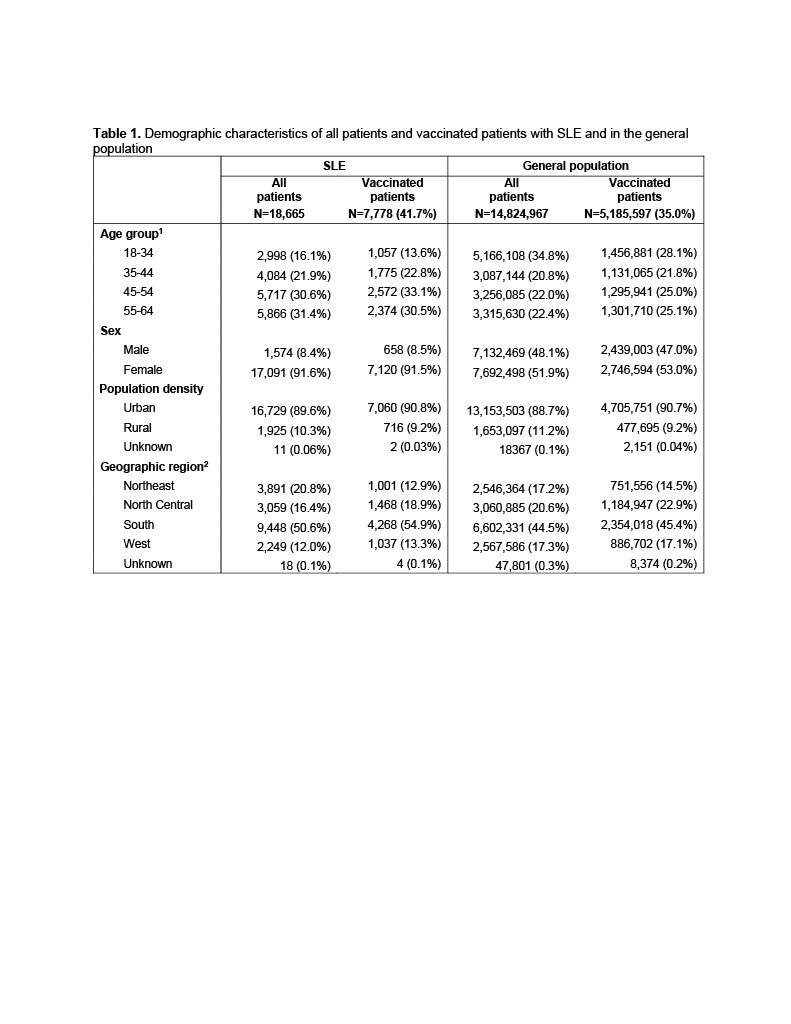
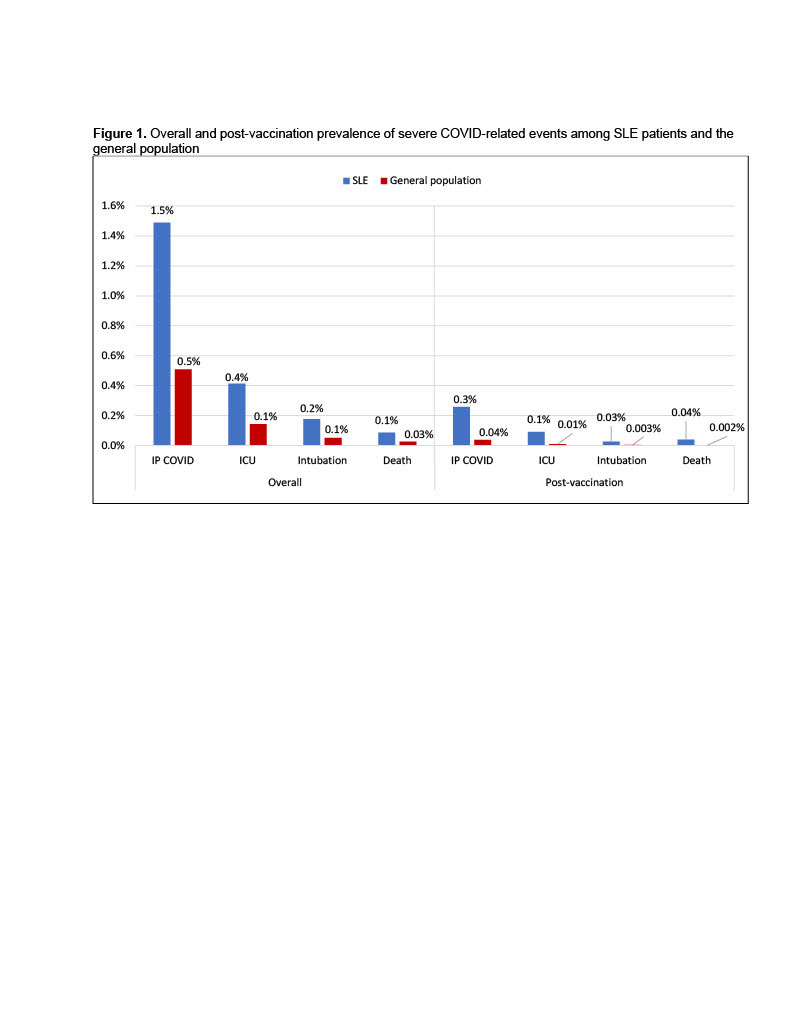
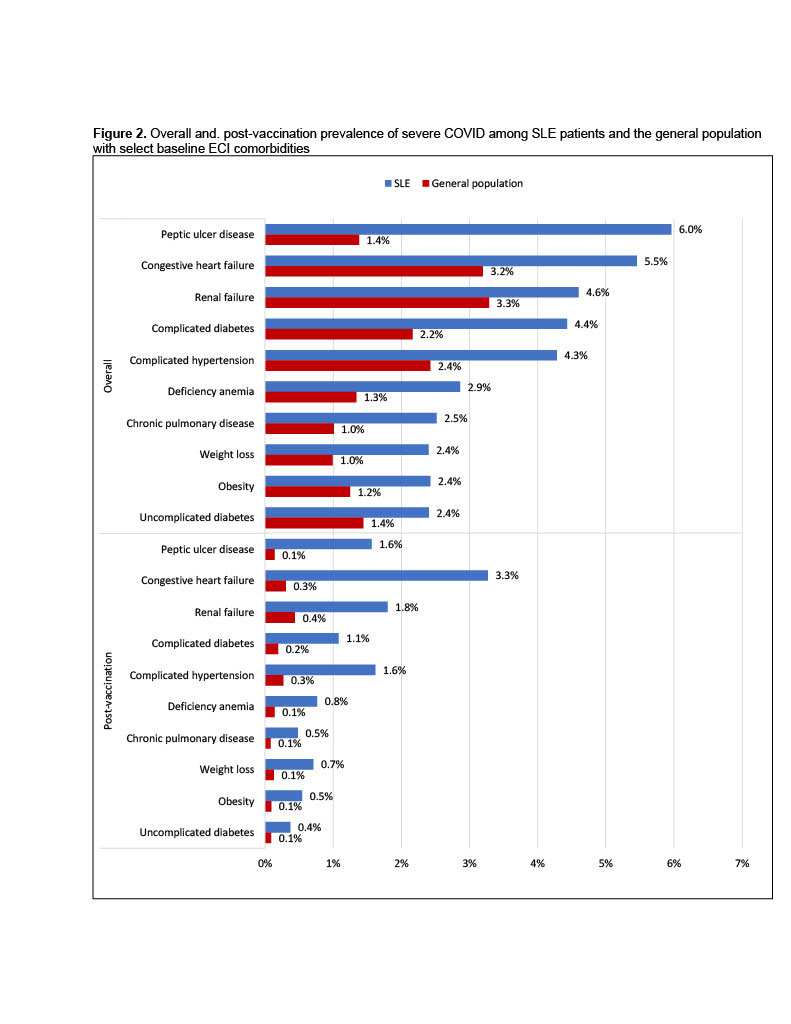
Results: 18,665 SLE patients and 14,824,967 patients in the general population met inclusion criteria (Table 1). Vaccination was more common among SLE patients vs. the general population (41.7% vs. 35.0%). Severe COVID rates, among those with COVID, were significantly higher in SLE than the general population overall (12.4% vs. 6.1%) and post-vaccination (7.6% vs. 2.2%). When reported at population level across all patients (Figure 1), severe COVID rates for SLE and the general population were 1.5% vs. 0.5% overall and 0.3% vs 0.04% post-vaccination. The overall rates and post-vaccination rates for COVID-related ICU, intubation and death were also significantly higher for SLE than the general population. Certain comorbidities were associated with increased risk of severe COVID, including peptic ulcer disease, congestive heart failure, renal failure, complicated diabetes and complicated hypertension, among others (Figure 2). Notably, SLE patients with peptic ulcer disease had much higher severe COVID rates than the general population (6.0% vs. 1.4% overall and 1.6% vs 0.1% post-vaccination). The post-vaccination severe COVID rate among SLE patients with congestive heart failure was disproportionally higher than those in the general population (3.3% vs 0.3%). All comparisons were significant (p< 0.01).
Conclusion: This study suggested a significantly increased risk in severe COVID for patients with SLE with a decreased prevalence in vaccinated patients. Certain comorbidities such as congestive heart failure among SLE pose additional risk factors for severe COVID outcomes. Preventative approaches, including vaccinations and other prophylaxis, to protect these at-risk SLE patients should continue to be encouraged.
To cite this abstract in AMA style:
Wu S, Atefi G, Moynihan M, Evans K, Palmer L, Pollack M, Dube C, Calabrese C. Overall and Post-vaccination Prevalence of Severe COVID-19-related Events Among Commercially Insured Patients with Systemic Lupus Erythematosus and the General U.S. Population [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/overall-and-post-vaccination-prevalence-of-severe-covid-19-related-events-among-commercially-insured-patients-with-systemic-lupus-erythematosus-and-the-general-u-s-population/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/overall-and-post-vaccination-prevalence-of-severe-covid-19-related-events-among-commercially-insured-patients-with-systemic-lupus-erythematosus-and-the-general-u-s-population/