Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic sclerosis (SSc) is a chronic autoimmune disorder which results in multi-organ dysfunction and high morbidity and mortality. There is limited data on healthcare resource usage in patients with SSc. The purpose of this study was to compare healthcare utilization among incident cases of SSc vs age- and sex-matched comparators without SSc.
Methods: A retrospective, population-based cohort of physician-diagnosed patients with SSc in a geographically well-defined area from Jan 1, 1988 to Dec 31, 2016 was assembled. Fulfillment of 2013 ACR/EULAR classification criteria for SSc was ascertained. A 2:1 cohort of age- and sex-matched non-SSc subjects from the same population base was randomly selected for comparison. Outpatient utilization data were obtained beginning 12 months prior to the SSc incidence/index date. Patients were followed until death, migration from the area, or December 31, 2017. A maximum of 5 years following the incidence/index date was used for analysis and the follow-up of each matched triple was further truncated at the shortest length of follow-up for any member, to ensure similar periods of observation for SSc cases and non-SSc comparators. Services were summarized as visit-days (number of days at least one service in the category was billed) to avoid overestimation of services provided. Utilization was compared between SSc and non-SSc cohorts using negative binomial and multinomial models.
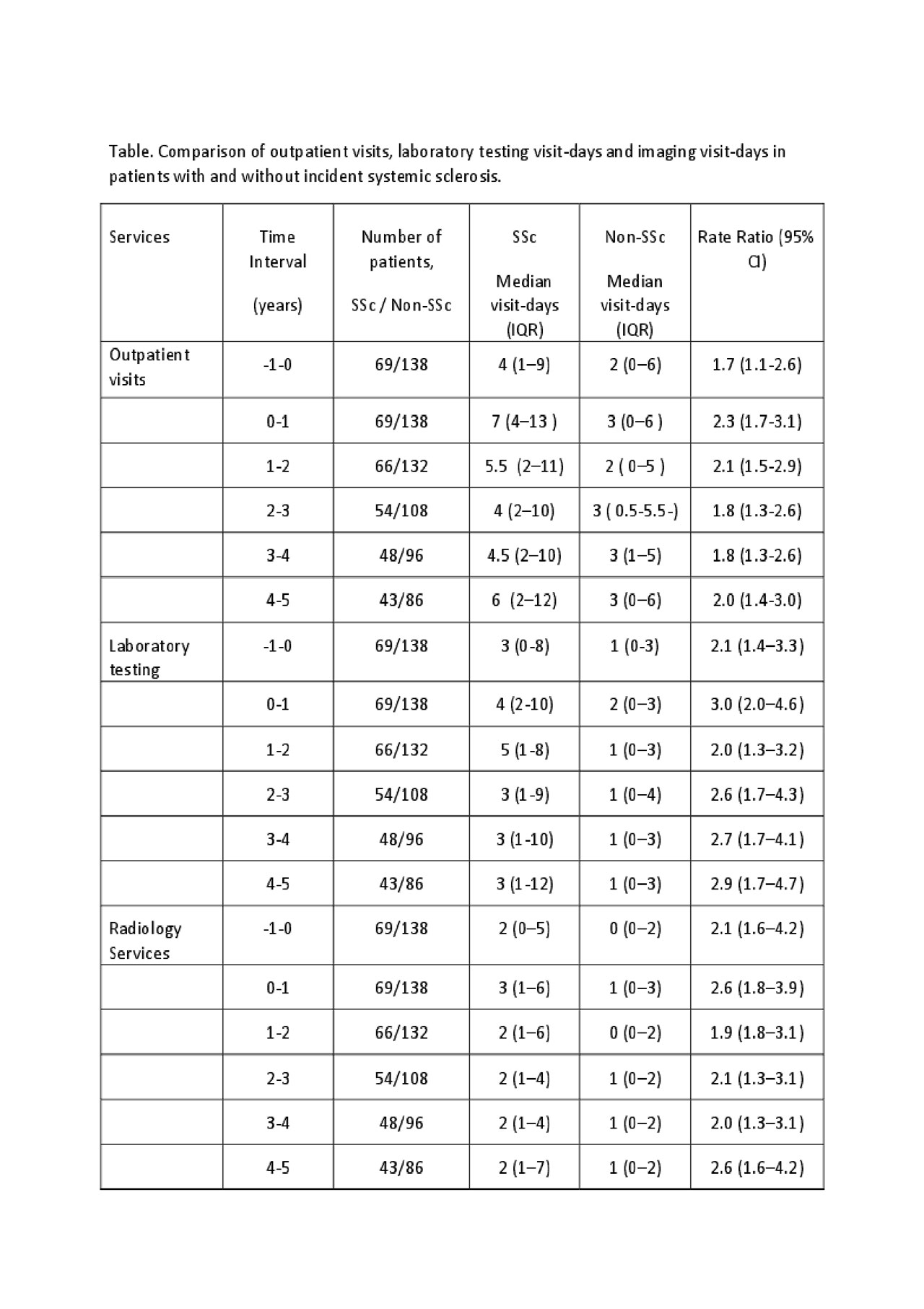
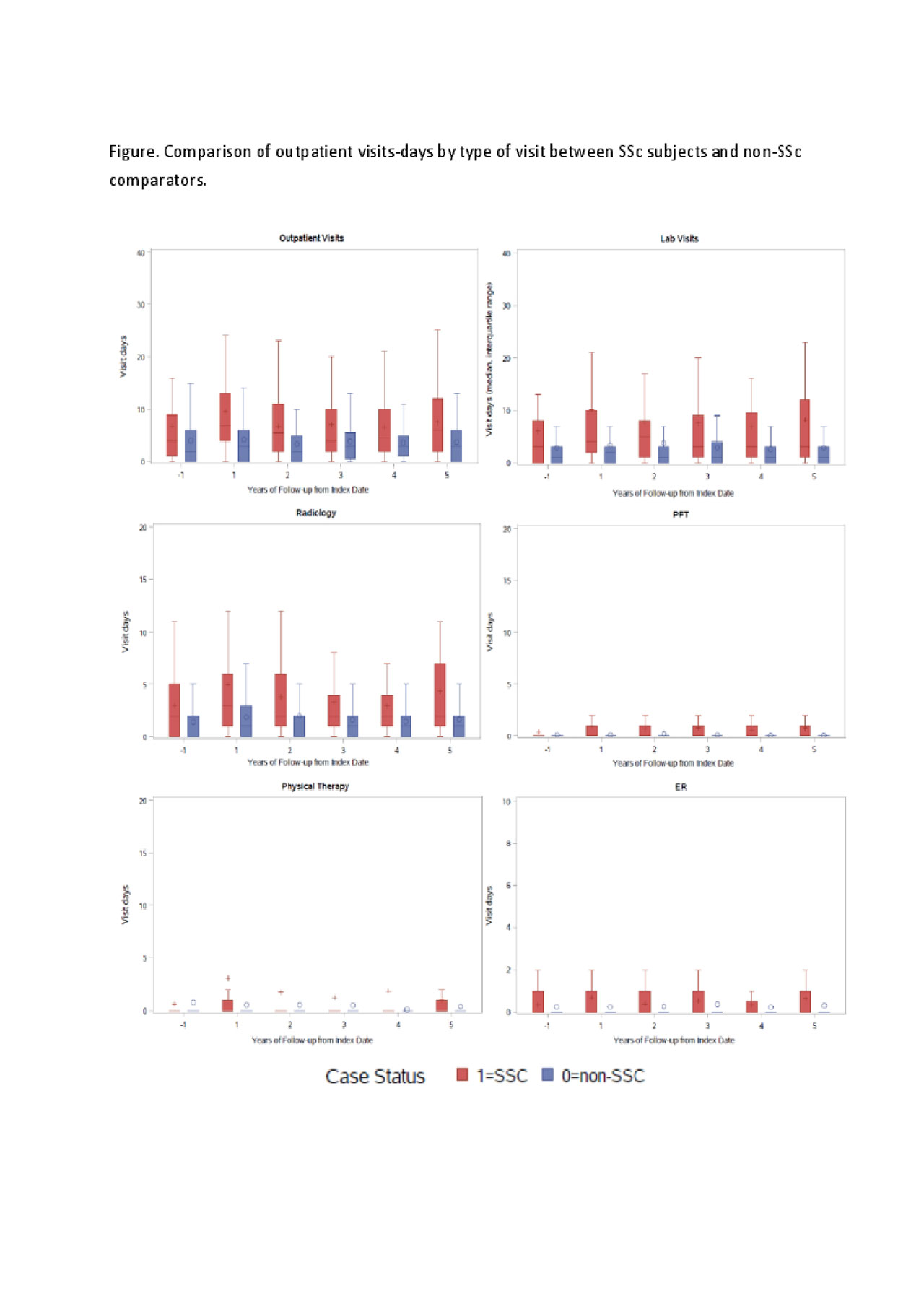
Results: The cohort included 69 incident SSc cases and 138 non-SSc comparators (mean age of 57 ± 16 years at diagnosis/index, 90% female for both cohorts; 87% [SSc] and 95% [non-SSc] Caucasian). Patients with SSc had the highest utilization of outpatient physician visit-days, laboratory visit-days and combined radiology visit-days during the year of the SSc diagnosis compared with the year prior to diagnosis or years 1 to 4 after diagnosis of SSc (Table, Figure). They also had higher utilization of outpatient physician, laboratory and combined radiology visit-days annually for the year prior to SSc diagnosis and for each of the first 5 years after SSc diagnosis compared to patients without SSc (Table). Rate ratios comparing utilization in patients with and without SSc ranged from 1.8 to 3.0 for all comparisons.
In the year of SSc diagnosis, visit-days specifically for X-rays, computed tomography scan, ultrasound, cardiovascular and gastroenterological testing and procedures, pulmonary function testing, emergency department visit, and physical therapy were higher for SSc subjects than non-SSc comparators, with rate ratios ranging from 2.5 to 13.0. Utilization of magnetic resonance imaging, nuclear medicine imaging, and musculoskeletal procedures were similar between groups in the year of diagnosis.
Conclusion: A higher utilization of outpatient physician visit-days, laboratory visit-days and radiology visit-days was observed among patients with SSc compared to non-SSc subjects throughout 5 years of disease duration, indicating high and continued care needs in this patient population. Highest utilization of services among SSc subjects occurred during the year of SSc diagnosis.
To cite this abstract in AMA style:
Coffey C, Sandhu A, Crowson C, Asante D, Matteson E, Osborn T, Warrington K, Makol A. Outpatient Healthcare Utilization Among Incident Cases of Systemic Sclerosis: Results from a Population-based Cohort (1988-2016) [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/outpatient-healthcare-utilization-among-incident-cases-of-systemic-sclerosis-results-from-a-population-based-cohort-1988-2016/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outpatient-healthcare-utilization-among-incident-cases-of-systemic-sclerosis-results-from-a-population-based-cohort-1988-2016/