Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with AAVs are typically on immunosuppression medications that might increase their risk of severe infections. COVID-19 has been associated with severe pulmonary manifestations among various disease populations. In this study, we aimed to explore the effects of COVID-19 on patients with AAV.
Methods: Using 2019-2020 National Inpatient Sample (NIS) data, COVID-19 hospitalizations were analyzed, distinguishing COVID-19 patients with AAV using the International Classification of Diseases – 10 Clinical Modification (ICD-10-CM) codes. The primary outcome was in-hospital mortality, and secondary outcomes included ICU admissions, acute kidney injury (AKI), acute respiratory failure (ARF), length of stay, and total hospital charge. Multivariate logistic regression and linear regression were used to adjust for common confounders such as sex, age, race, steroid and immunomodulator use, and further renal and respiratory comorbidities.
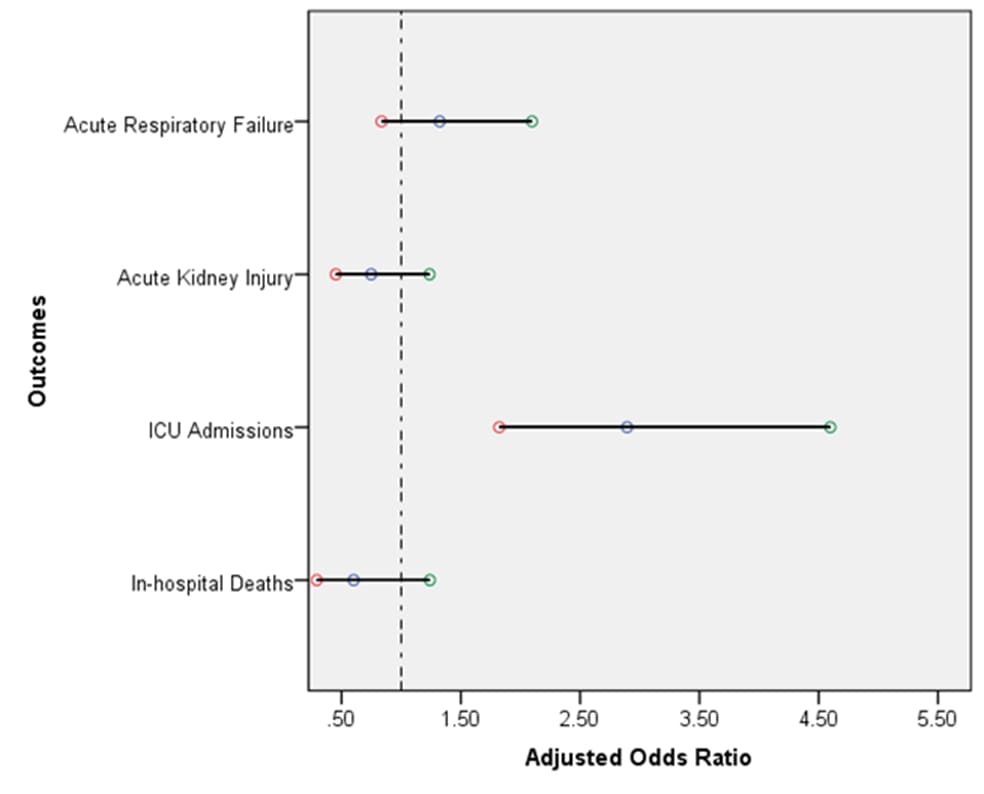
Results: Of the 1,018,405 COVID-19 hospitalizations, 545 had an AAV diagnosis. The mean age for the AAV population was 61 years, meanwhile 64.7 years for the general COVID-19 population without an AAV diagnosis (p=0.0064). Among the AAV patients, females represented 47% vs 53% of males (p=0.15). After adjusting for potential confounding, individuals with an AAV diagnosis exhibited no statistically significant adjusted odds ratios (aOR) for in-hospital mortality (aOR of 0.6, 95% CI: 0.29-1.2, p= 0.16). Additionally, there was no statistically significant difference in the odds of having AKI (aOR of 0.74, 95% CI: 0.45-1.23, p= 0.25) and ARF (aOR of 1.3, 95% CI: 0.83-2.09, p= 0.23). However, they had significantly higher odds for ICU admissions compared to those without. (aOR of 3.1, 95% CI: 1.9-4.9, p < 0.0001). The mean length of stay was longer in patients with AAV (10.5 days vs 7.4 days for those without), and their total hospital charge was higher (122305 dollars vs 78711 dollars). Significant disease baseline characteristics include higher odds of being on chronic steroids and having CKD.
Conclusion: Our results demonstrate that the outcomes of in-hospital mortality, AKI, and ARF among AAV patients infected with COVID-19 are similar to those of the general population despite increased ICU admissions, length of stay, and total hospital charges.
To cite this abstract in AMA style:
El Sharu H, Mubaydeen T, Romero Noboa M. Outcomes of COVID-19 in Patients with ANCA-Associated Vasculitis (AAV) [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/outcomes-of-covid-19-in-patients-with-anca-associated-vasculitis-aav/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-covid-19-in-patients-with-anca-associated-vasculitis-aav/