Session Information
Date: Saturday, November 7, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes I: Morbidity (0980–0984)
Session Type: Abstract Session
Session Time: 5:00PM-5:50PM
Background/Purpose: Antimalarial medications (AMs) are central to the management of SLE, affording numerous clinical benefits including the reduction of disease flare. However, little is known about the effects of AM withdrawal in patients who have achieved prolonged disease quiescence. We aimed to investigate the rate of flare in lupus patients who withdrew their AM after achieving clinical remission for at least one year, compared to those who continued therapy. Furthermore, we aimed to compare flare rates in cases who tapered AM versus abruptly withdrew.
Methods: Using the University Lupus Clinic long-term observational cohort study database, we identified 1573 lupus patients ever treated with AM. Cases were defined as those who achieved clinical remission for at least one year then ceased their AM (n = 165). Index date was defined as the date of complete AM cessation. Controls were defined as patients who achieved clinical remission for at least one year and continued AM. Controls were matched according to the duration of antimalarial therapy before the start of clinical remission and the duration of therapy from remission date to case index date (Figure 1). All patients were required to have at least two years of follow up. Of 96 cases with adequate follow up, 88 were successfully matched to one control and 85 to a second control, resulting in a near 1:2 match. In total, there were 88 cases and 173 controls.
Results: Patient characteristics for cases (withdrew AM) and controls (continued AM) are presented in Table 1. Disease flare occurred in 61.4% of cases compared to 45.1% of controls (p = 0.002, Figure 2). The most common types of flare were skin and musculoskeletal flares. Reasons for AM withdrawal included self-cessation (feeling well, pregnancy, medication concerns), toxicity (retinal, mucocutaneous, cardiac), disease quiescence or other reasons such as side effects requiring investigation. Retinal toxicity as defined by the SLICC damage index occurred in 1.9% of patients. Over half of patients who withdrew AM later restarted it, typically due to disease flare. Following recommencement for flare, most patients (88%) recaptured control or improved, while 12% had further flares. Regarding patients who withdrew AM, 42% tapered and 58% ceased abruptly (Table 1). The median duration (months) spent on AM from one year after clinical remission to cessation was expectedly longer in the taper group (29.2 months) compared to the abrupt withdrawal group (11.2 months). Patients who tapered had significantly fewer flares (45.9%), similar to the rate for controls (45.1%), when compared to those who withdrew abruptly (72.6%; p = 0.01, Figure 2). Additionally, fewer patients in the taper group restarted AM following cessation (37.8%) compared to the abrupt withdrawal group (62.7%; p = 0.02).
Conclusion: Antimalarial medications aid in preventing disease flare even in patients who have achieved prolonged clinical remission. For those who withdraw therapy, tapering results in lower rates of disease flare, similar to those seen in patients who continue AMs. Hence, except in the setting of toxicity, cessation of antimalarial therapy in patients with prolonged disease quiescence is feasible using a slow taper.
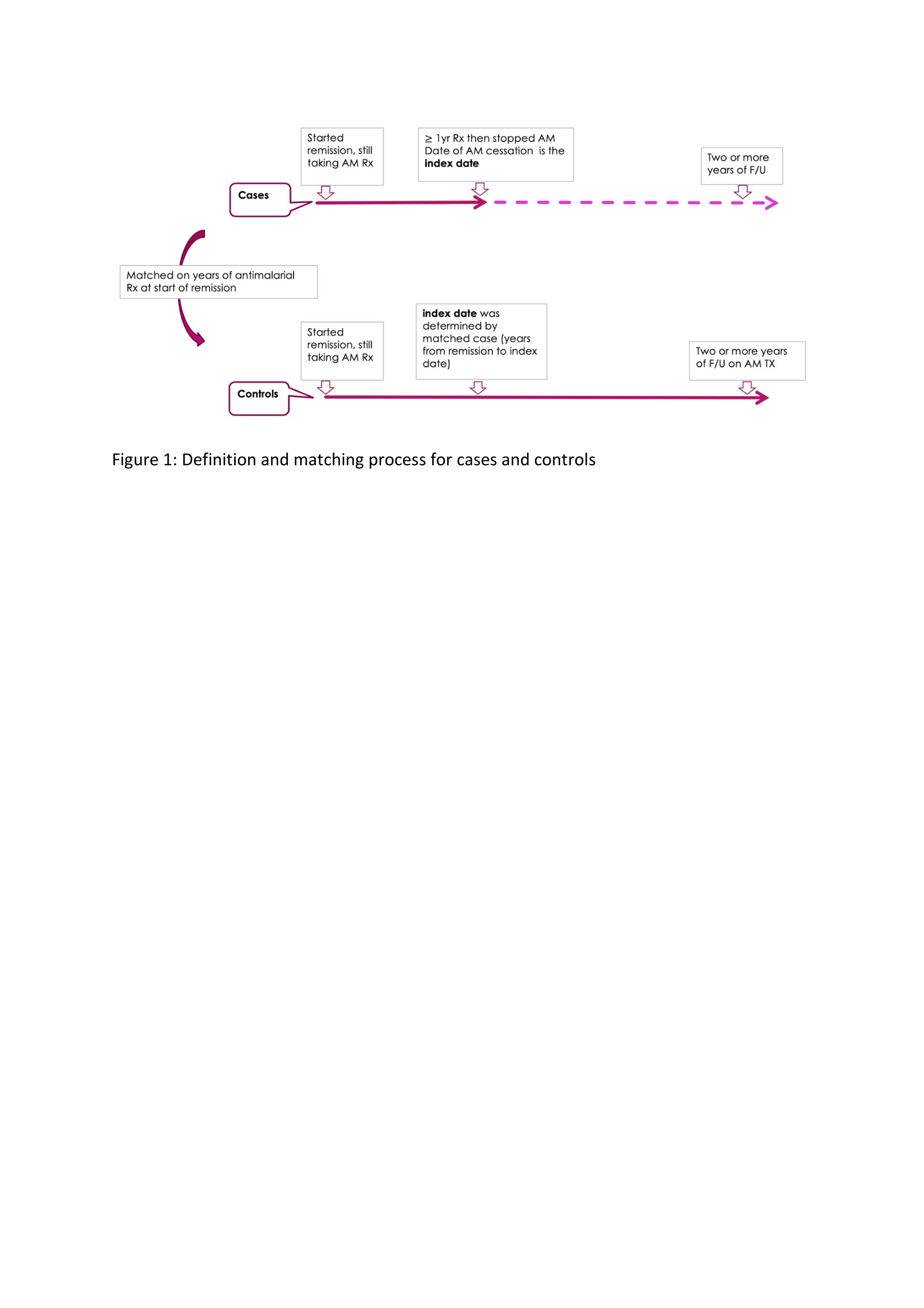 Figure 1: Definition and matching process for cases and controls
Figure 1: Definition and matching process for cases and controls
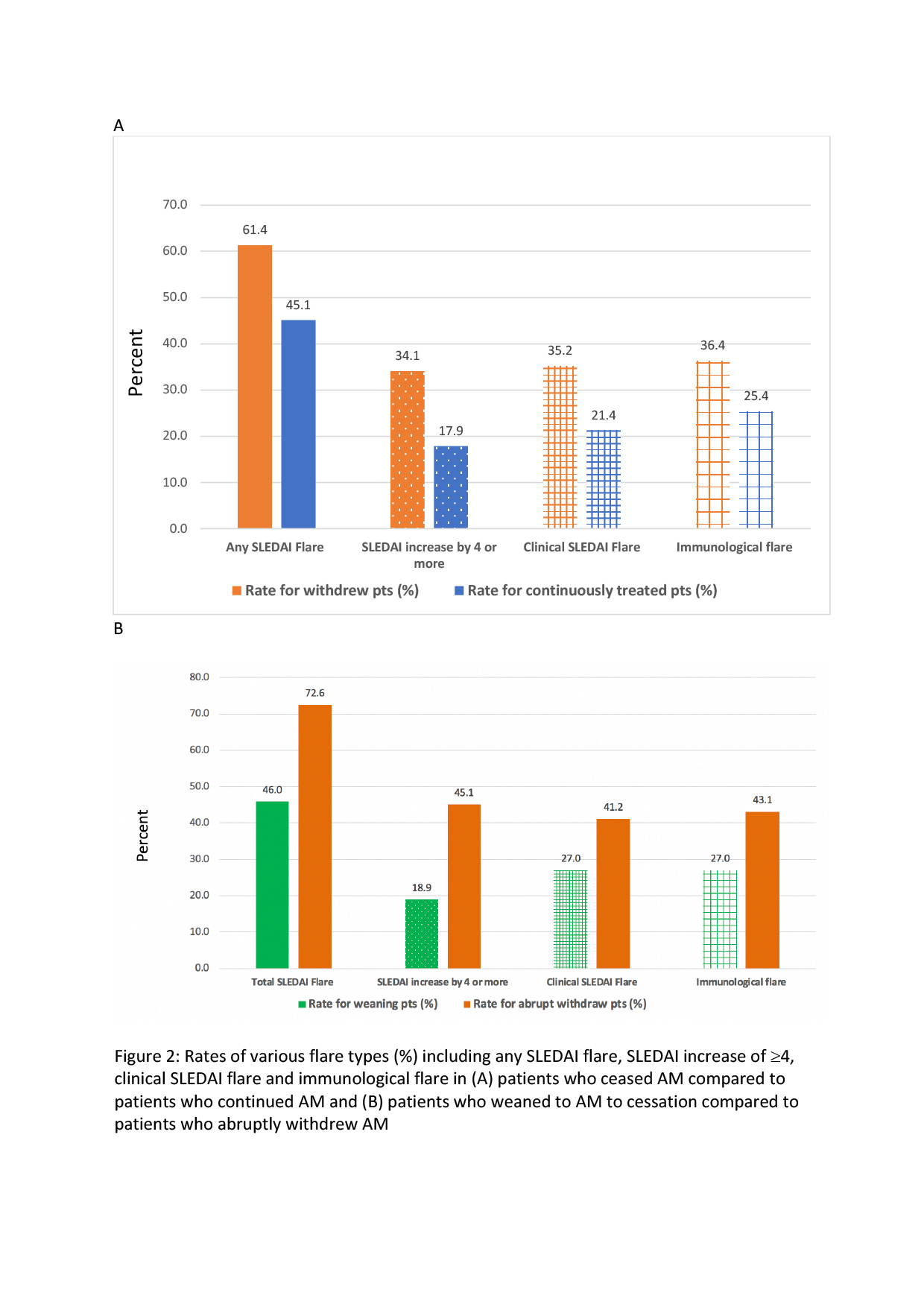 Figure 2: Rates of various flare types (%) including any SLEDAI flare, SLEDAI increase by 4 or more, clinical SLEDAI flare and immunological flare in (A) patients who ceased AM compared to patients who continued AM and (B) patients who weaned to AM to cessation compared to patients who abruptly withdrew AM
Figure 2: Rates of various flare types (%) including any SLEDAI flare, SLEDAI increase by 4 or more, clinical SLEDAI flare and immunological flare in (A) patients who ceased AM compared to patients who continued AM and (B) patients who weaned to AM to cessation compared to patients who abruptly withdrew AM
To cite this abstract in AMA style:
Papachristos D, Gladman D, Su J, Urowitz M. Outcomes Following Antimalarial Withdrawal in Patients with Quiescent Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/outcomes-following-antimalarial-withdrawal-in-patients-with-quiescent-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-following-antimalarial-withdrawal-in-patients-with-quiescent-systemic-lupus-erythematosus/

