Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic Lupus Erythematosus (SLE) is an autoimmune inflammatory disease associated with an increased risk of cardiovascular complications, including acute coronary syndrome (ACS). However, there is limited real-world data available to comprehensively analyze the outcomes of ACS in patients with SLE over an extended period. This study aimed to compare the characteristics and outcomes of hospitalized patients with ACS, stratified by the presence or absence of SLE. The primary outcome was to examine the inpatient mortality, hospital length of stay, total hospital charges.
Methods: A retrospective observational analysis was conducted utilizing data from the US National Inpatient Sample (NIS) spanning the period from 2006 to 2019. Patients admitted with a diagnosis of ACS were categorized into two groups: those with International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and -10) codes defining SLE and those without any SLE code. Demographics, clinical characteristics, and comorbidities were recorded. Furthermore, outcomes such as in-hospital mortality, complications, length of stay, and total hospital charges were analyzed and compared between the two groups. Associations between SLE and specific morbidity were assessed using chi-square tests, while t-tests were employed for continuous variables.
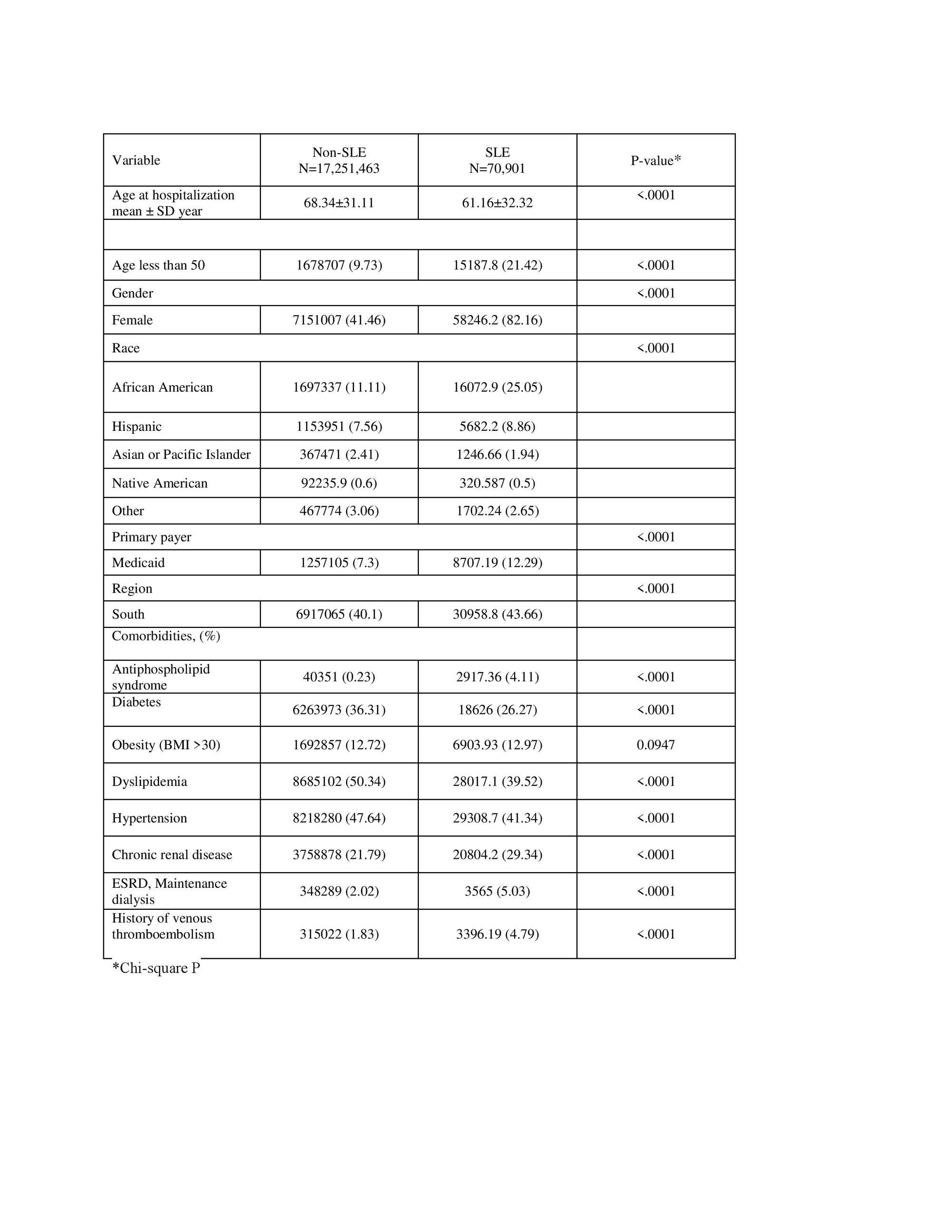
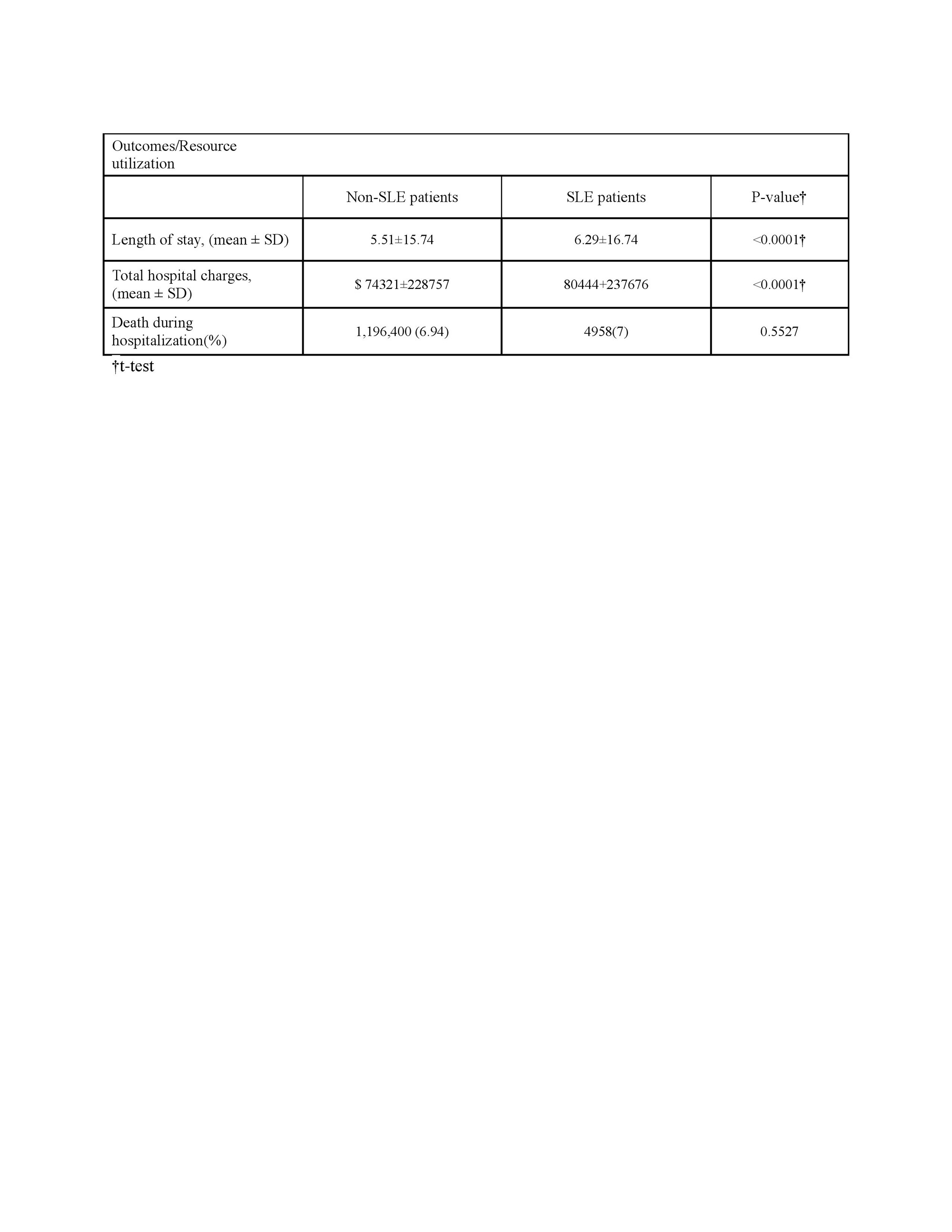
Results: A total of 17,322,365 (adjusted for sampling weight) ACS hospitalizations were identified in the NIS database, of which 70,901 (0.41%) were in patients with SLE (Table 1). Patients with SLE were more likely to be younger (mean age 61 vs 68 years; p < 0.0001), under 50 (21% vs 9%), female (82% vs 41%), and African American (25% vs 11%) compared to non-SLE patients. In addition, SLE patients were more statistically significant to have Medicaid (12% vs 7; p< 000.1) and live in the Southern region of the USA (43% vs 40%, p< 0.0001). Regarding comorbidities, SLE patients with ACS exhibited a higher prevalence of certain conditions, including antiphospholipid syndrome, chronic renal disease, ESRD and a history of thromboembolism (Table 1). Conversely, non-SLE patients with ACS had higher rates of comorbidities such as diabetes, hypertension, and dyslipidemia. Significant differences were observed in outcomes and resource utilization (Table 2). ACS in SLE patients was associated with longer length of stay (mean 6.2 vs 5.5 days; p< 0.0001) and higher cost (mean total charges $80,444 vs $74,321; p < 0.0001). No difference in the in-patient mortality was observed among the 2 groups.
Conclusion: Patients with SLE and ACS were younger, more likely to be female and African American. In addition, hospitalization of SLE patients with ACS is associated with longer hospital stay, and higher total cost compared to non-SLE. Further research is needed to optimize the prevention and management of ACS in the SLE population.
To cite this abstract in AMA style:
Parperis K, Bhattarai B. Outcomes and Clinical Features of Acute Coronary Syndrome in Patients with SLE: A 14-Year Real-World Study (2006-2019) [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/outcomes-and-clinical-features-of-acute-coronary-syndrome-in-patients-with-sle-a-14-year-real-world-study-2006-2019/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-and-clinical-features-of-acute-coronary-syndrome-in-patients-with-sle-a-14-year-real-world-study-2006-2019/