Session Information
Date: Monday, October 27, 2025
Title: (1467–1516) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Past reports have shown that serositis is a risk factor for organ damage in patients with SLE. However, the distinct clinical features of newly onset SLE with serositis remain unclear. This study aims to elucidate specific clinical features of SLE with serositis at initial onset compared to those without.
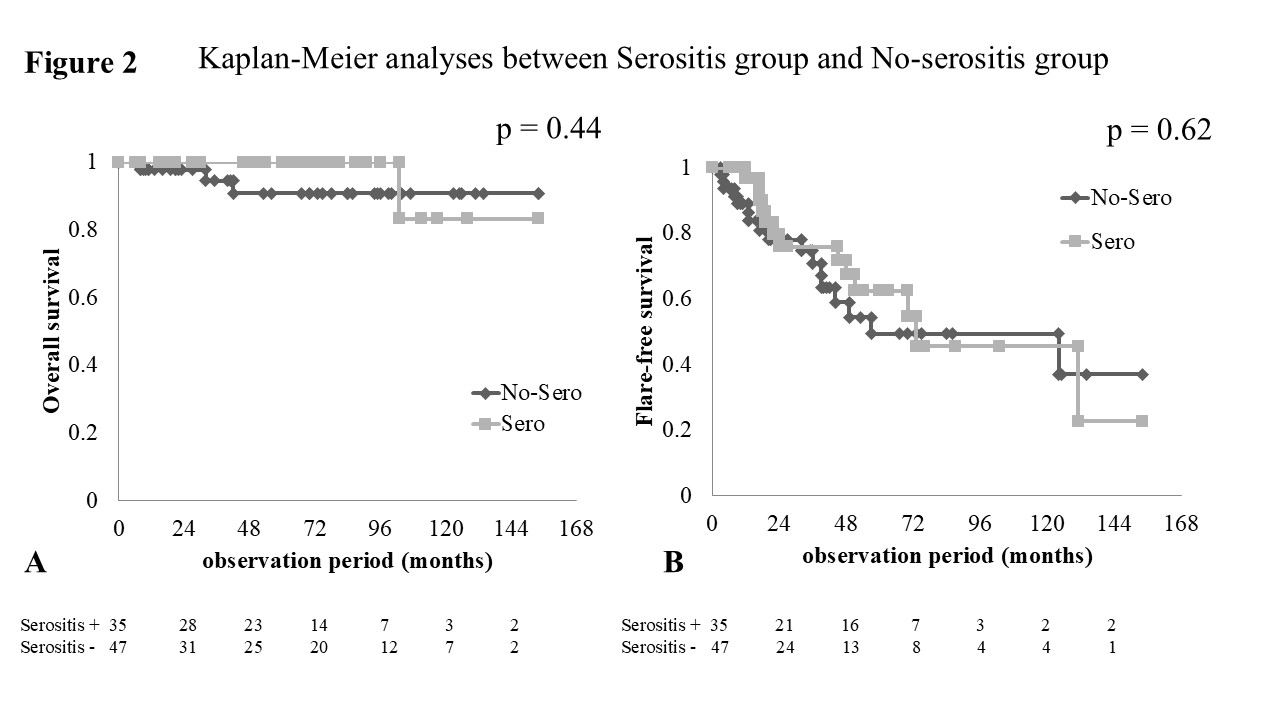
Methods: This study is a retrospective inception cohort design. Newly diagnosed patients with SLE treated in the Department of Rheumatology at Fukushima Medical University Hospital between 2011 and 2023 were included. Patients who followed up for over 6 months were selected for this study. Those with newly onset SLE with serositis, which includes pericarditis, pleuritis, and peritonitis, were classified as the serositis group. Clinical features, including age, sex, disease duration, SLE symptoms, laboratory data, disease activity, organ damage, and treatment, were compared with those without serositis (no-serositis group). Cumulative overall survival and flare-free survival were also compared between the two groups using Kaplan-Meier analysis.
Results: Among 95 patients with newly onset SLE treated in our department, 82 patients were included. The mean age was 36.5 years, and 75 patients were female (91.8%). The mean observation period was 61.9 months, and the mean SLEDAI score was 18.4. Among the 82 patients, 35 (42.7%) had serositis at the initial disease onset. The comparison of clinical characteristics between the serositis group (35 patients) and no-serositis group (47 patients) is shown in Figure 1. General characteristics were similar between the two groups, except for higher SLEDAI scores and lower complement levels in the serositis group. The serositis group showed a significantly increased number of flares with serositis compared to no-serositis group. Additionally, the SDI scores at the end of follow-up were significantly higher in the serositis group. In terms of therapy, significantly higher PSL doses and increased frequencies of mPSL pulse therapy were observed in the serositis group. Kaplan-Meier analysis revealed similar cumulative overall and flare-free survival rates between the two groups (Figure 2). We further analyzed the risk factors for organ damage accrual (SDI of 1 or more) in patients with newly onset SLE. Logistic regression analysis indicated that age and serositis were independent risk factors for damage accrual (odds ratio: age 1.05, 95%CI 1.01-1.09; serositis 2.74, 95%CI 1.01-7.40, respectively, p< 0.05).
Conclusion: Newly onset SLE with serositis may demonstrate higher organ damage accrual compared to that without serositis. More frequent flare-ups of serositis/enteritis may occur in newly onset SLE with serositis.
 Clinical features of newly-onset SLE patients with serositis compared to those without
Clinical features of newly-onset SLE patients with serositis compared to those without
.jpg) Kaplan-Meier analyses between newly-onset SLE with serositis group and those without (no-serositis group)
Kaplan-Meier analyses between newly-onset SLE with serositis group and those without (no-serositis group)
To cite this abstract in AMA style:
Sato S, Moriuchi K, Yamamoto S, Nibu H, Sakamoto T, Ogawa S, Saito K, Sumichika Y, Yoshida S, Matsumoto H, Temmoku J, Asano T. Outcome of Newly Diagnosed SLE with Serositis and Its Clinical Features in Daily Clinical Practice: A Single Center Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/outcome-of-newly-diagnosed-sle-with-serositis-and-its-clinical-features-in-daily-clinical-practice-a-single-center-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcome-of-newly-diagnosed-sle-with-serositis-and-its-clinical-features-in-daily-clinical-practice-a-single-center-study/
