Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Opioid use disorder (OUD) is associated with high morbidity and mortality and in the U.S. in 2022, resulted in over 81,000 overdose deaths.1 However, little is known about the prevalence of OUD in patients with rheumatic disease (RMD). Medications for OUD (MOUD; buprenorphine, methadone, naltrexone) are known to reduce mortality in OUD, yet no study has examined the use of MOUD in patients with RMD. This study had two primary objectives: to describe the population of patients with RMD with and without OUD and to assess use of MOUD in this population.
Methods: The data source used in this study was the All of Us Research Program (version 8), a national cohort consisting of electronic medical records for > 393,000 enrolled U.S. adults. We identified those with >2 ICD-9/10 or SNOMED codes for RA, SLE, spondyloarthritis (SpA), or osteoarthritis < 2 years pre-enrollment. Patients with OUD were identified with >1 ICD 9/10 or SNOMED code for opioid dependence or abuse that occurred after the first code for RMD. Demographic characteristics (race, age at enrollment, sex at birth, insurance type), prevalent psychiatric disorders (bipolar disorder, schizophrenia, schizoaffective disorder, borderline personality disorder, depression, anxiety, and post-traumatic stress disorder), Charleson comorbidity index (CCI), and acute care utilization (emergency department [ED] visits, hospitalizations) < 1 year prior to first OUD code were compared between patients with RMD with and without OUD. We identified a subset of patients with OUD codes and no prior MOUD use at any point prior to the first OUD code and examined differences in patient characteristics between those who received MOUD vs. did not in the subsequent period.
Results: Among 37,282 patients with RMD, we identified 1,502 (4%) with OUD billing codes (Table 1). Patients with vs. without OUD were younger, had more comorbidities, had higher acute care utilization, were more likely to have Medicaid insurance, and had a higher prevalence of psychiatric diagnoses, including psychotic and mood disorders. Patients with vs. without OUD were more likely to have RA, SLE, and SpA diagnoses. MOUD was initiated in 163/1121 (14.5%) patients. Patients who received vs did not receive MOUD were younger (mean (SD) age 55.6 (12.3) p = 0.003), had fewer comorbidities (CCI (SD) 2.6 (2.6) vs 3.3 (3.1) p = 0.001) more likely to be male (42.9% vs 27.7% p < 0.001), and were more likely to have PTSD (14.1% vs 8.7% p = 0.04).
Conclusion: In this nationwide population with RMD, we found demographic, clinical and psychiatric differences among patients with RMD with vs. without OUD. General population estimates of MOUD are around 25%, which is higher than in this RMD population.1 Future research is needed to understand the barriers that exist for patients with RMD and OUD to receiving MOUD, the influence of social risk factors on development and treatment of OUD, and the role of increased screening for psychiatric disorders with comorbid OUD and RMD. References1. Dowell D, Brown S, Gyawali S, et al. Treatment for Opioid Use Disorder: Population Estimates — United States, 2022. MMWR Morb Mortal Wkly Rep. 2024;73(25):567-574. doi:10.15585/mmwr.mm7325a1
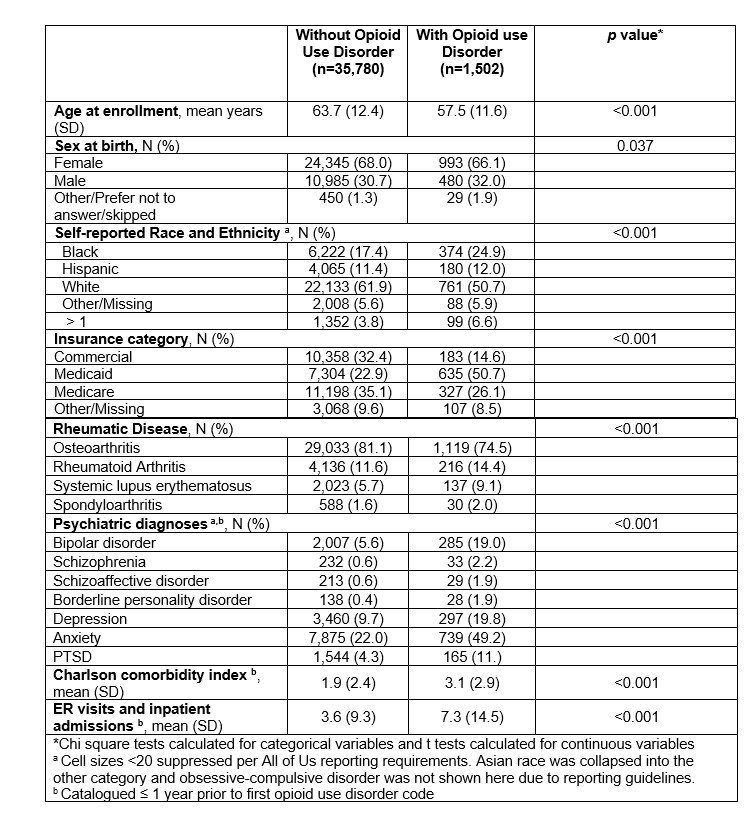 Table 1. Characteristics of patients with RMD in the All of Us Research Program (version 8) by the presence of opioid use disorder
Table 1. Characteristics of patients with RMD in the All of Us Research Program (version 8) by the presence of opioid use disorder
To cite this abstract in AMA style:
Riegler J, Santacroce L, Costenbader K, Feldman C. Opioid Use Disorder Among Patients with Rheumatic Conditions in the All of Us Research Program: A Descriptive Analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/opioid-use-disorder-among-patients-with-rheumatic-conditions-in-the-all-of-us-research-program-a-descriptive-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/opioid-use-disorder-among-patients-with-rheumatic-conditions-in-the-all-of-us-research-program-a-descriptive-analysis/
