Session Information
Date: Sunday, November 17, 2024
Title: Abstracts: Systemic Sclerosis & Related Disorders – Clinical I
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Lung transplantation (LT) is a potentially life-saving treatment for patients with systemic autoimmune rheumatic diseases (SARDs) who have developed end-stage lung disease due to interstitial lung disease (ILD). Although double lung transplant (DLT) has been associated with better graft survival than single lung transplant (SLT) in patients with idiopathic pulmonary fibrosis (IPF), lungs are a scarce resource. Thus, to offer LT to a greater number of patients, transplant centers also perform SLT in patients with IPF and other forms of ILD, including SARD-ILD. However, it is unknown whether DLT confers a survival benefit over SLT in patients with SARD-ILD. The primary aim of this study was to determine whether adults with SARD-ILD have higher 1-year mortality rates after SLT than after DLT. We hypothesized that SLT would be associated with higher 1-year mortality rates than DLT among adults with SARD-ILD.
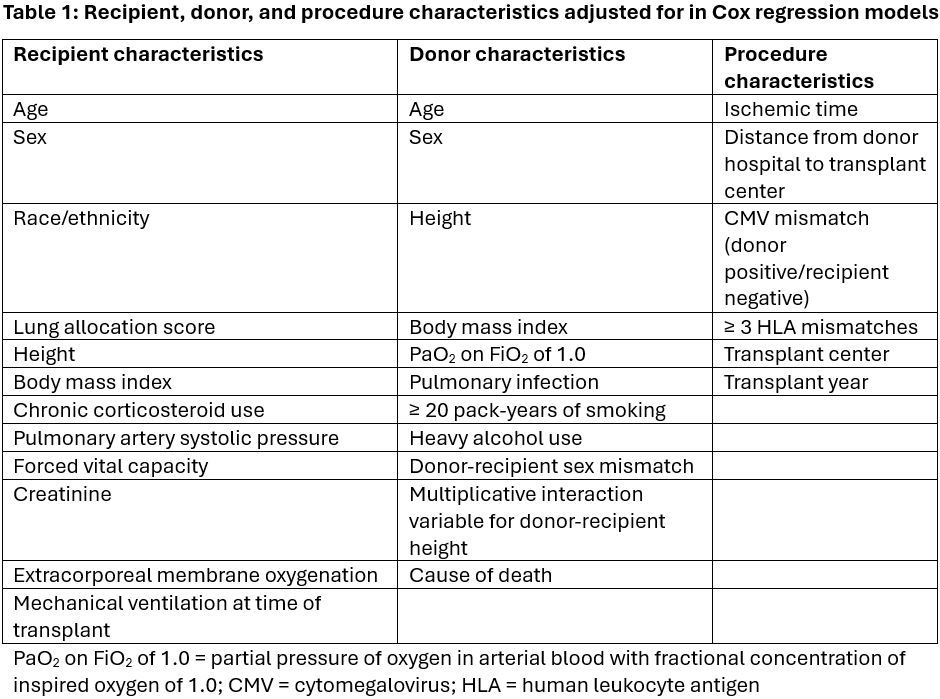
Methods: We performed a retrospective cohort study of adults who underwent DLT or SLT in the United States between May 4, 2005 (the date of implementation of the lung allocation score system) and December 31, 2019. Data were provided by the United Network for Organ Sharing, a non-profit organization that records data on all solid organ transplants performed in the United States. Subjects were included if they were at least 18 years of age at the time of LT, underwent a DLT or SLT during the study period, and had a diagnosis of a SARD. Subjects were excluded if they had received a heart-lung transplant, if they received a LT from a living donor, or if they had missing data on diagnosis or survival time. We modeled transplant procedure type (DLT vs. SLT) as the independent binary variable of interest in stratified Cox models where survival time was the dependent variable, adjusting for recipient, donor, and procedure factors (Table 1). We used multiple imputation to account for missing covariate data.
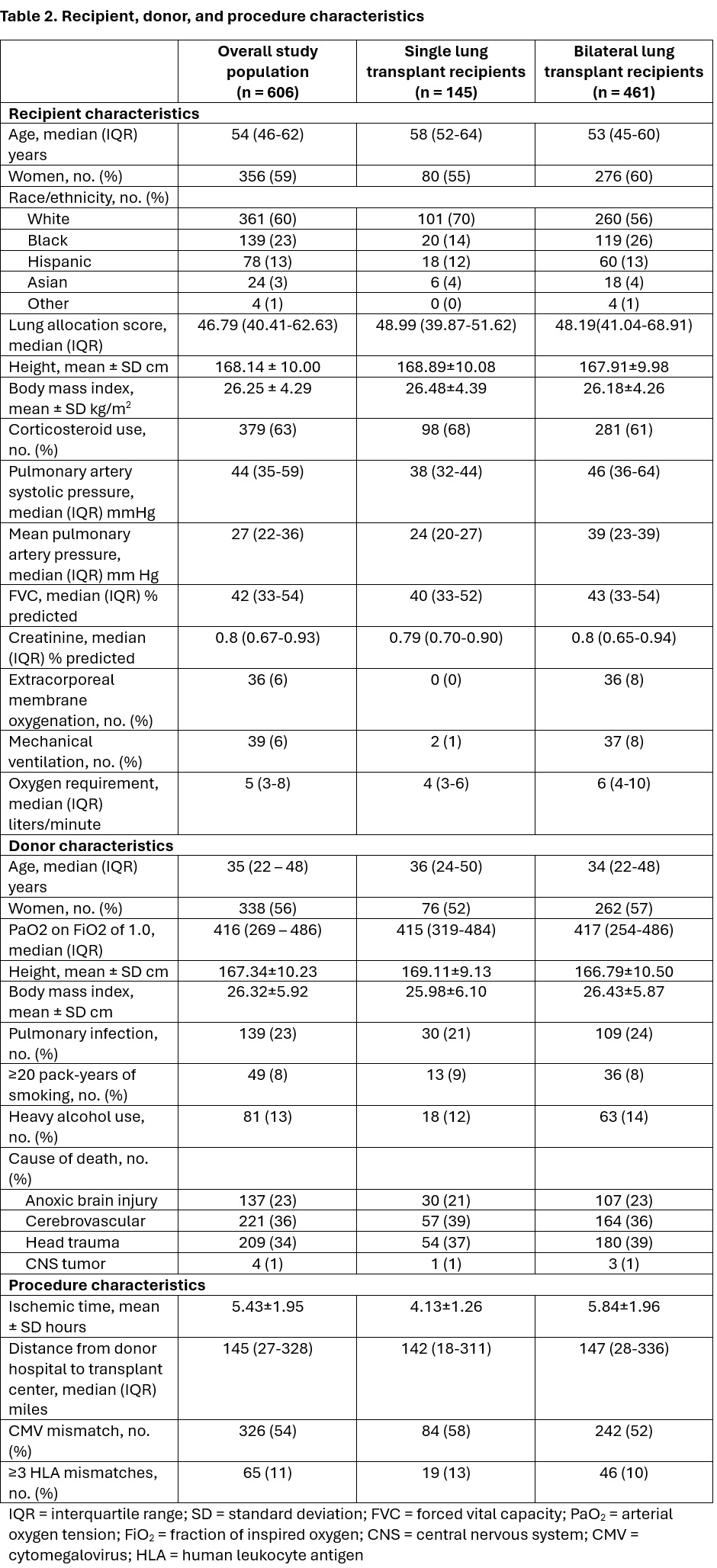
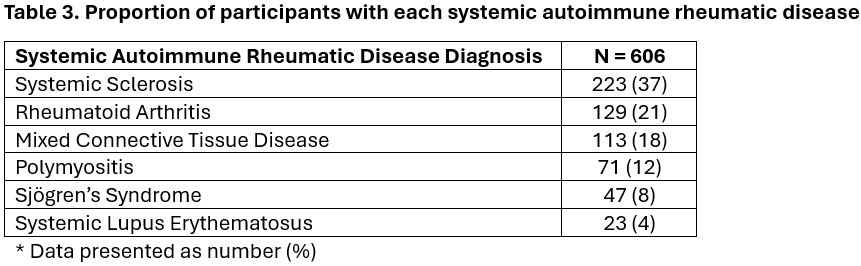
Results: Six-hundred six adults with SARD-ILD were transplanted during the study period and met inclusion criteria. The median (interquartile range) age was 54 (46-62) years; 59% were female (Table 2). The majority (76%) underwent DLT. The breakdown of SARD diagnoses is included in Table 3; a plurality (37%) had systemic sclerosis . The 1-year unadjusted mortality rate following LT per 100 person-years was 14.97 among those who underwent DLT and 17.24 among those who underwent SLT. In an unadjusted model, SLT was not associated with a relative increase in 1-year mortality compared to DLT (hazard ratio [HR] 1.19, 95% confidence interval [CI] 0.75 to 1.19, p = 0.46). Likewise, in our fully adjusted model – adjusted for recipient, donor, and procedure factors – SLT was not associated with a relative increase in the 1-year mortality rate compared to DLT (HR 1.49, 95% CI 0.34 to 6.57, p = 0.60).
Conclusion: Adults with SARD-ILD who underwent SLT did not have an increased risk of death at 1 year compared to those who underwent DLT. Offering SLT to appropriately selected adults with SARD-ILD who require LT is a reasonable transplant strategy and will result in a greater number of available lungs to transplant to SARD-ILD patients in need.
To cite this abstract in AMA style:
Hurley H, Benvenuto L, Bernstein E. One-Year Survival Following Single versus Double Lung Transplantation in Adults with Systemic Autoimmune Rheumatic Disease-related Interstitial Lung Disease: A Nationwide Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/one-year-survival-following-single-versus-double-lung-transplantation-in-adults-with-systemic-autoimmune-rheumatic-disease-related-interstitial-lung-disease-a-nationwide-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/one-year-survival-following-single-versus-double-lung-transplantation-in-adults-with-systemic-autoimmune-rheumatic-disease-related-interstitial-lung-disease-a-nationwide-cohort-study/