Session Information
Date: Monday, November 8, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Outcomes (1257–1303)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Up to 40% of individuals with lupus nephritis (LN) develop chronic kidney disease (CKD). Biopsy studies have revealed that patients with SLE can have active class III, IV, or V LN even in the absence of proteinuria or an abnormal glomerular filtration rate (GFR). We hypothesized that some patients with LN might be classified as treatment responders based on proteinuria, yet continue to accrue kidney damage. We sought to characterize early CKD in LN, and assessed the ability of traditional prognostic features, such as renal biopsy class and resolution of proteinuria, to identify patients likely to accrue progressive renal damage.
Methods: We conducted a single center retrospective study of SLE patients diagnosed with their first episode of biopsy-proven class III, IV, and/or V LN (n = 37). Participants with fewer than five years of clinical follow-up data were excluded, as were participants diagnosed with LN before 2004, so as to reflect modern outcomes. For each participant, eGFR calculated by CKD-EPI was graphed over time from date of renal biopsy to five years thereafter. Participants were divided into those with progressive GFR loss (GFR slope < -5 mL/min/1.73 m2 per year) versus those who maintained a stable GFR (GFR slope not meeting the above threshold). Baseline demographics, renal biopsy features, immunologic status, treatment regimen, and comorbidities were compared between GFR trajectory groups using the Student’s t-test, Wilcoxon rank-sum test, or Fisher’s exact test as appropriate. Finally, proteinuria was assessed at one year after renal biopsy, and participants were classified as complete responders if urine protein was < 500 mg/mg at this time.
Results: Among these participants diagnosed with their first episode of LN, 30% (n = 11) accrued progressive renal damage despite standard of care therapy over the first five years following renal biopsy (Figure 1). There were no significant differences in baseline characteristics between GFR trajectory groups, including no association between progressive GFR loss and renal biopsy class, chronicity index, prednisone dosage, induction regimen, ACE inhibitor or ARB initiation, or prevalence of pre-existing hypertension or diabetes (Table 1). Likewise, resolution of proteinuria at one year did not differentiate between GFR trajectory groups (Table 2). Notably, 55% of participants with progressive GFR loss (n = 6 of 11) would be classified as complete responders based on < 500 mg/mg urine protein at one year after biopsy, and 33% (n = 6 of 18) of complete responders based on this urine protein threshold continued to accrue renal damage.
Conclusion: We have identified an understudied category of patients with LN who accrue progressive renal damage despite apparent response to standard of care therapy. Roughly half of the participants in this study with a worrisome GFR trajectory would be misleadingly classified as complete responders at one year based on resolution of proteinuria. These findings indicate that definitions of LN treatment response based on proteinuria can fail to identify patients who continue to accrue renal damage despite treatment. Better definitions and biomarkers of response are needed to improve long-term renal outcomes and trial design.
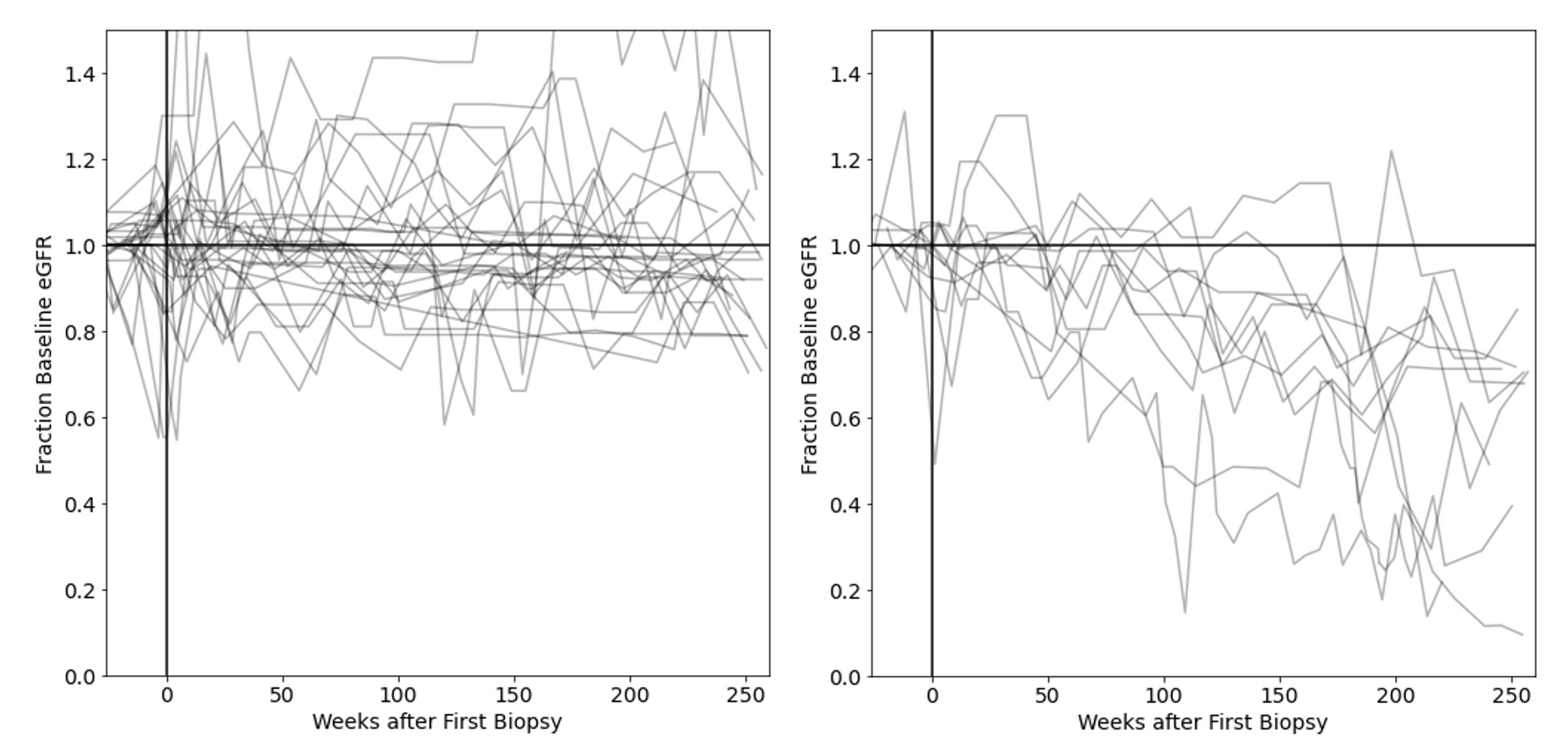 Figure 1. GFR trajectories of participants who maintained a stable GFR (left panel; n = 26) versus those who progressively lost GFR (right panel; n = 11). Each line represents the GFR values for one participant over time. To facilitate comparison between participant trajectories, GFR values were normalized to each participant’s pre-LN baseline GFR.
Figure 1. GFR trajectories of participants who maintained a stable GFR (left panel; n = 26) versus those who progressively lost GFR (right panel; n = 11). Each line represents the GFR values for one participant over time. To facilitate comparison between participant trajectories, GFR values were normalized to each participant’s pre-LN baseline GFR.
 Table 1. Baseline or other early characteristics of the GFR trajectory groups. Unless otherwise noted, average values are shown.
Table 1. Baseline or other early characteristics of the GFR trajectory groups. Unless otherwise noted, average values are shown.
 Table 2. Response status (based on proteinuria < 500 mg/mg) at one year versus GFR trajectory group. Resolution of proteinuria at one year did not associate with ultimate GFR trajectory (p = 1.0). Response status could not be calculated for two participants in the stable GFR group (excluded from this table) due to missing clinical information at one year.
Table 2. Response status (based on proteinuria < 500 mg/mg) at one year versus GFR trajectory group. Resolution of proteinuria at one year did not associate with ultimate GFR trajectory (p = 1.0). Response status could not be calculated for two participants in the stable GFR group (excluded from this table) due to missing clinical information at one year.
To cite this abstract in AMA style:
Weeding E, Fava A, Goldman D, Petri M. One Third of Lupus Nephritis Patients Classified as Complete Responders Continue to Accrue Progressive Renal Damage Despite Resolution of Proteinuria [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/one-third-of-lupus-nephritis-patients-classified-as-complete-responders-continue-to-accrue-progressive-renal-damage-despite-resolution-of-proteinuria/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/one-third-of-lupus-nephritis-patients-classified-as-complete-responders-continue-to-accrue-progressive-renal-damage-despite-resolution-of-proteinuria/
