Session Information
Date: Monday, November 11, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster II: Treatments, Outcomes, & Measures
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose:
Patients with rheumatoid arthritis (RA) experience premature mortality that is largely due to cardiovascular disease (CVD). Ample evidence suggests that elevated γGT activity is associated with increased risk of CVD. Our aim was to assess the determinants of increased γGT activity in patients with RA, focusing on markers of disease activity and cardiovascular risk factors.
Methods:
Cross-sectional study including successive RA patients hospitalized in the Rheumatology department of Cochin Hospital for a 12-month period. Data on liver function, disease activity, hepatotoxic and cardiovascular risk factors were systematically collected and all patients were assessed by Power Doppler Ultrasound (PDUS) performed on 32 joints. DAS28-γGT was calculated by replacing ESR by γGT in the following formula: 0.56*√TJ-28+0.28*√SJ-28+2*ln (γGT)+0.014*GH
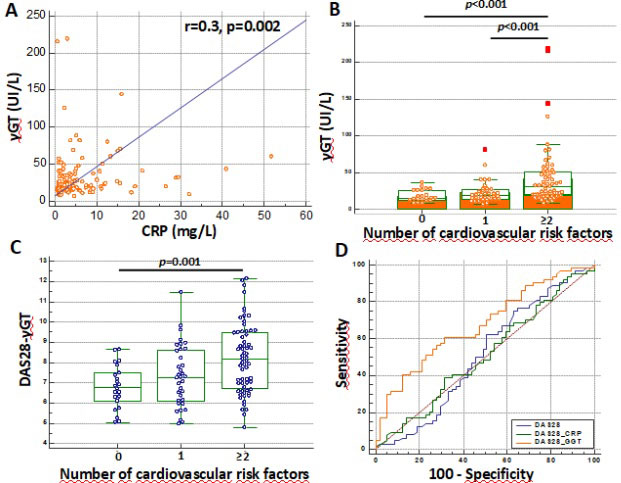
Results: We included 124 patients: 85% were women and mean age was 58 years. Thirty-one patients (25%) had isolated γGT increase. γGT correlated with CRP (r=0.30, p=0.002) (Figure 1A). No correlation was observed between γGT and ESR, DAS28 or DAS28-CRP. γGT were significantly increased in patients with alcohol consumption (median (range): 35 (20-144) UI/L vs. 22 (7-219) UI/L, p=0.012), type 2 diabetes mellitus (35 (8-215) UI/L vs. 21 (7-219) UI/L, p=0.024), blood hypertension (35 (8-215) UI/L vs. 21 (7-219) UI/L, p=0.024), dyslipidemia (28 (7-219) UI/L vs. 19 (8-215) UI/L, p=0.004) and metabolic syndrome (48 (14-219) UI/L vs. 21 (7-144) UI/L). γGT levels gradually increased with the number of cardiovascular risk factors (p< 0.001) (Figure 1B). In multivariate analysis, γGT levels > 35 UI/L was associated with CRP > 10 mg/L (OR : 4,88, 95% CI 1,59-15,03) and the presence of dyslipidemia (OR: 3.13, 5% CI 1.09-8.97).
Given that γGT reflected both systemic inflammation and metabolic condition, we constructed a composite index called DAS28- γGT to test the merit of this marker for the global evaluation of RA. DAS28- γGT remains a reliable marker of RA disease activity which correlated with DAS28 (r=0.50, p< 0.001), DAS28-CRP (r=0.70, p< 0.001), ESR (r=0.30, p< 0.001), CRP (r=0.50, p< 0.001), global OMERACT-EULAR synovitis Score on PDUS (r=0.22, p=0.024) and HAQ (r=0.35, p< 0.001). Patients with blood hypertension (median (range) 8.16 (5.41-12.14) vs 7.26 (4.80-11.47) p=0.012), dyslipidemia (8.24 (4.80-12.14) vs. 7.08 (5.04-11.81), p=0.011) and metabolic syndrome (8.47 (6.23-12.03) vs. 6.40 (4.80-12.14)) were more likely to have increased DAS28-γGT. Conversely to the DAS28 and DAS28-CRP, DAS28-γGT steadily increased according to the number of cardiovascular risk factors (Figure 1C), and had a diagnostic value for the presence of at least 2 cardiovascular risk factors characterized by an AUC of 0.70 (p< 0.001) compared to 0.51 for DAS28 and DAS28-CRP (Figure 1D)
Conclusion:
Our results support that γGT levels may be considered as markers of systemic inflammation, metabolic syndrome and cardiovascular risk in patients with RA. We propose an original index, the DAS28-γGT, able to evaluate both disease activity and cardiovascular risk. This index would deserve further validation in prospective cohorts.
To cite this abstract in AMA style:
Vergneault H, Vandebeuque E, Codullo V, Allanore Y, Avouac J. One Size Fits All : Replacing ESR by γGT in DAS28 Calculation Permits a Dual Evaluation of Joint Activity Together with Cardiovascular Risk [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/one-size-fits-all-replacing-esr-by-%ce%b3gt-in-das28-calculation-permits-a-dual-evaluation-of-joint-activity-together-with-cardiovascular-risk/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/one-size-fits-all-replacing-esr-by-%ce%b3gt-in-das28-calculation-permits-a-dual-evaluation-of-joint-activity-together-with-cardiovascular-risk/