Session Information
Date: Friday, November 6, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes Poster I: Multimorbidity
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Despite frequent reports of sleep problems, accurate information on sleep disturbance in rheumatoid arthritis (RA) is not available. Studies using objective measures of sleep in RA are rare, but are needed to provide greater accuracy than classifications based on self-report. We examined the presence and severity of obstructive sleep apnea (OSA) using a validated home-monitoring device among Individuals with RA.
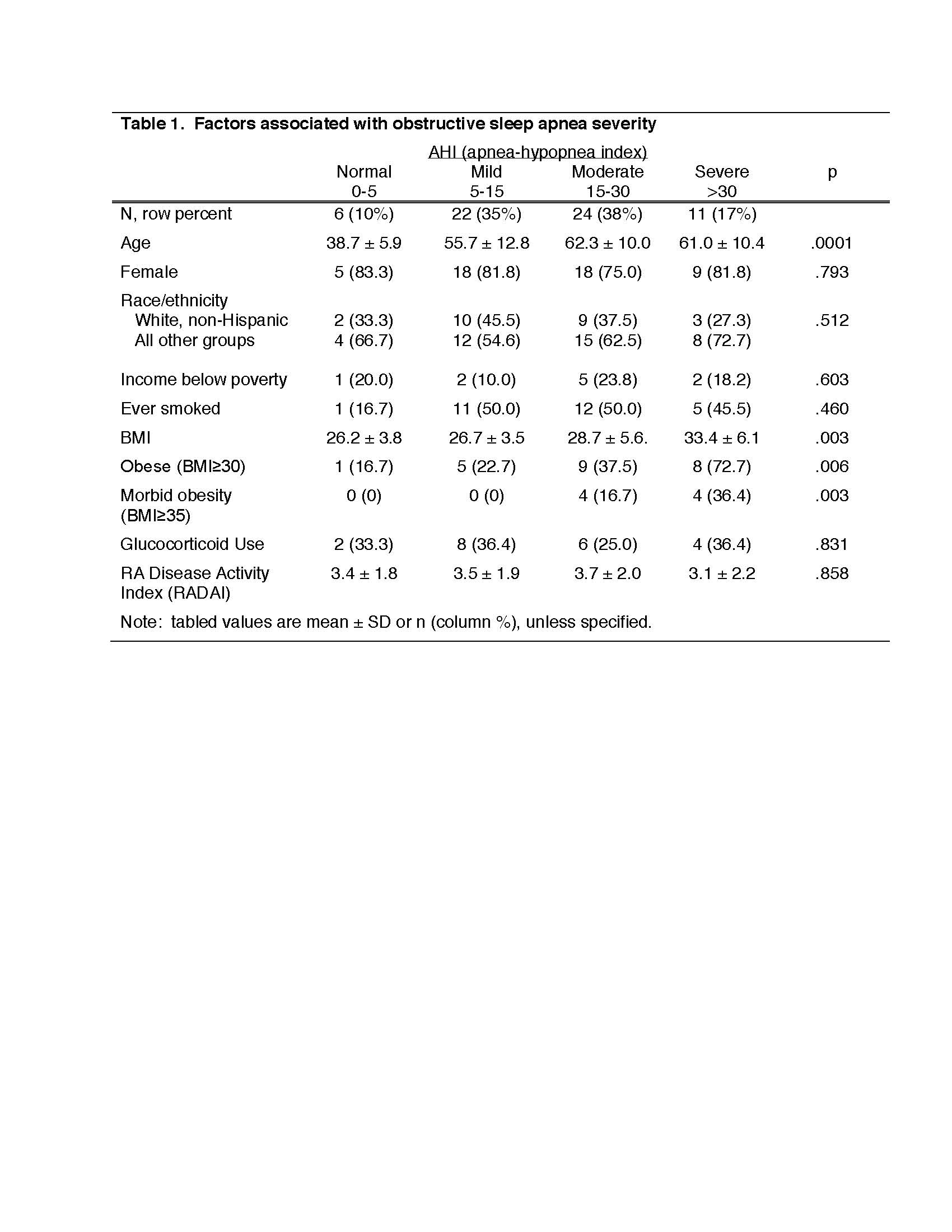
Methods: Data were from the RA Sleep Study, in which participants were recruited from an academic medical center and a safety-net hospital clinic. They completed in person visits and questionnaires every 6 months over an 18-month period and interviews were conducted in Spanish and English. All have physician-diagnosed RA; current use of a CPAP device was an exclusion criterion. At baseline, participants were provided with a WatchPAT™ device (Itamar Medical, Ltd) to wear for two consecutive nights at home. The WatchPAT™ is a validated diagnostic wrist-worn device which measures multiple channels of data (peripheral arterial tone, oximetry, actigraphy, heart rate and chest motion) with 3 points of contact (wrist, finger, and chest sensor). It yields estimates on a variety of measures, including the apnea-hypopnea index (AHI), reflecting the number of apnea or hypopnea episodes per hour of sleep. AHI was categorized as normal (< 5), mild OSA (5- < 15), moderate OSA (15-< 30), or severe OSA (≥30). The STOP-BANG questionnaire1, a validated measure of OSA risk was also administered and physician diagnoses of OSA were queried. Potential predictors of the presence and severity of OSA were identified through chi-square test and analysis of variance with post-hoc means comparisons, and included age, sex, race/ethnicity (white non-Hispanic vs. all others), smoking, low income, BMI, obesity (BMI ≥ 30 kg/m2), morbid obesity (BMI ≥ 35), glucocorticoid use, and self-reported RA disease activity (Rheumatoid Arthritis Disease Activity Index, RADAI).
Results: Participants (n=63) were 79% female, 38% white non-Hispanic, 16% low income and mean age was 58 ± 13 years. Using AHI, OSA was frequent: 35% had mild OSA, 38% moderate, and 17% severe. Participants with normal AHI were significantly younger, and those with severe OSA had significantly higher BMI (Table 1). Among 13 (21%) participants identified as high risk for OSA in the STOP-BANG questionnaire, 6 (10%) reported a physician’s diagnosis of OSA. None of the participants with normal AHI had either a diagnosis of OSA or identified as high risk for OSA. (Table 2).
Conclusion: Some degree of sleep apnea was identified in 90% of this group of individuals with RA, with over half having moderate to severe OSA. Most OSA was unrecognized and would not be identified with current screening measures. OSA is linked to multiple health problems, including cardiovascular disease and fatigue, both of which are common in RA. Results highlight the importance of future objective studies of sleep as well as the importance of considering OSA as a risk factor for poor outcomes in RA.
1 Chung F et al. Anesthesiology 2008; 108:812-21
To cite this abstract in AMA style:
Rush S, Morsi S, Pinzón Tirado J, Trupin L, Stone K, Katz P. Objectively-Measured Obstructive Sleep Apnea Is Frequent Among Individuals with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/objectively-measured-obstructive-sleep-apnea-is-frequent-among-individuals-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/objectively-measured-obstructive-sleep-apnea-is-frequent-among-individuals-with-rheumatoid-arthritis/