Session Information
Date: Tuesday, November 7, 2017
Title: Rheumatoid Arthritis – Clinical Aspects Poster III: Comorbidities
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The links between inflammation, obesity and joint dysfunction are well established. How these translate into clinical disease activity and functional disability in rheumatoid arthritis (RA) though, remains to be defined. This study explores associations between BMI and 1. The achievement of disease remission or low disease activity and 2. Functional ability, in RA.
Methods: Data from two consecutive UK multi-centre RA inception cohorts with similar design were used: the Early RA Study (ERAS) and Early RA Network (ERAN). Recruitment figures/median follow up for ERAS and ERAN were 1465/10 years (maximum 25 years), and 1236/6 years (maximum 10 years) respectively. Standard demographic and clinical variables were recorded at baseline and then annually until loss to follow-up or the end of study follow up. Multivariable logistic regression analysis was used with remission (R-DAS)/low disease activity status (L-DAS) and health assessment questionnaire (HAQ, <1 vs ≥1) as dependent categorical variables in models adjusted for patient, disease-related clinical variables and recruitment year. BMI was examined in separate models as both a continuous and categorical predictor variable according to WHO definitions.
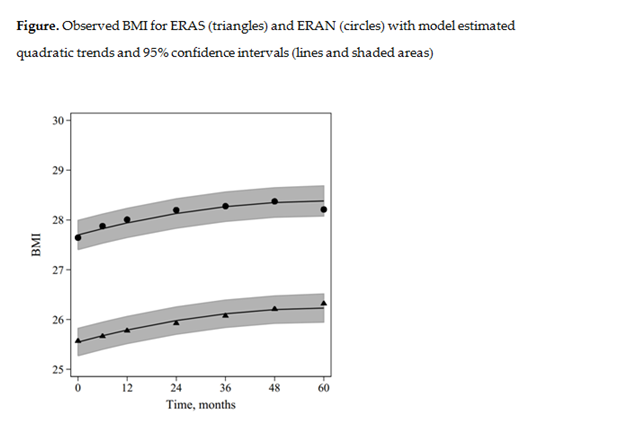
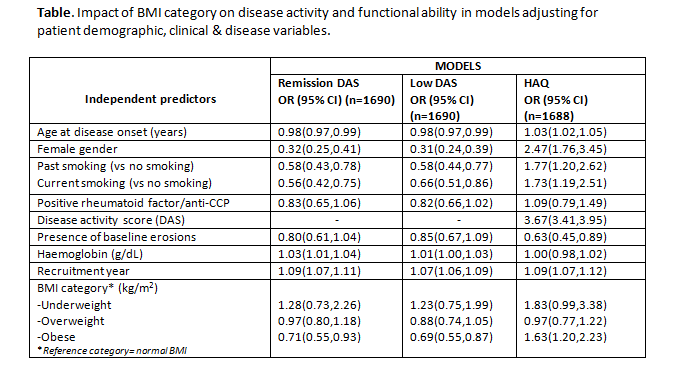
Results: Baseline BMI data from 2420 patients (90%) indicated that 37.2% were overweight, 21.3% obese. Mean BMI at baseline was 25.5 in ERAS and 27.6 in ERAN and this increased over 5 years (Figure). In multilevel logistic models (table) adjusting for age, sex and year of recruitment among other, higher BMI was associated with reduced odds of achieving R-DAS (OR 0.97;95%CI 0.95, 0.99) (table) and L-DAS, although the latter did not reach statistical significance (OR 0.98;95%CI0.96, 1.00). Obesity was related to a significantly lower chance of R-DAS by 29% (OR 0.71;95%CI 0.55, 0.93) and L-DAS by 31% (OR 0.69;95%CI 0.55,0.87). Higher BMI was predictive of higher disability (OR 1.04;95%CI 1.01,1.06). More specifically, obesity increased the odds of higher disability by 63% (OR 1.63;95%CI 1.20,2.23) and in the same models, higher DAS was also strongly predictive of higher disability (OR 3.67;95%CI 3.41,3.95).
Conclusion: Higher BMI and in particular obesity was associated with lower remission and low disease activity states and higher disability. These findings argue strongly for the screening and management of obesity to become a central part of all treatment strategies in RA.
To cite this abstract in AMA style:
Nikiphorou E, Norton S, Kiely P, Young A. Obesity and the Impact on Treat to Target Goals and Functional Ability in RA. Results from Two Multi-Centre UK Inception Cohorts [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/obesity-and-the-impact-on-treat-to-target-goals-and-functional-ability-in-ra-results-from-two-multi-centre-uk-inception-cohorts/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/obesity-and-the-impact-on-treat-to-target-goals-and-functional-ability-in-ra-results-from-two-multi-centre-uk-inception-cohorts/