Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Date: Thursday, April 30, 2020
Title: Poster Session 1
Session Type: ACR Abstract Session
Session Time: 6:00PM-7:00PM
Background/Purpose: Juvenile idiopathic arthritis (JIA) is the most common rheumatic disease in children. The use of infrared thermal imaging for screening JIA has not utilized standardized image analysis for population screening. Our group developed a standardized algorithm for region of interest (ROI) definition in lower extremities for children, which could be translated for evaluating JIA. In addition, we hypothesize that by using an internal reference such as mid tibia, the increased temperature of inflamed nearby joints (knees, ankles) can be reliably detected by thermal imaging.
Methods: Children with clinically active arthritis in knee and/or ankle and healthy controls were enrolled. All subjects underwent infrared thermal imaging of lower extremities. Patients in the arthritis group also had a joint exam performed by a pediatric rheumatologist and ultrasound examination. Arthritis was defined as swelling or limitation plus tenderness on exam. Joint effusion or tenosynovitis on ultrasound was the confirmation for joint or tendon inflammation. Infrared thermal data were analyzed using custom software with standardized ROI selection for knees, ankles and midtibia. Median and 95th percentile temperatures were recorded for each leg segment. Temperature after within-limb calibration (TAWiC) was defined as the temperature differences between joint and midtibia on the same leg. Absolute temperature and TAWiC were compared in joints with versus without arthritis using generalized estimating equations to account for lack of independence between left and right legs. Receiver operating characteristic (ROC) curve analysis was performed to determine area under the curve (AUC) and threshold for optimal sensitivity and specificity based on maximizing the sum of sensitivity and specificity.
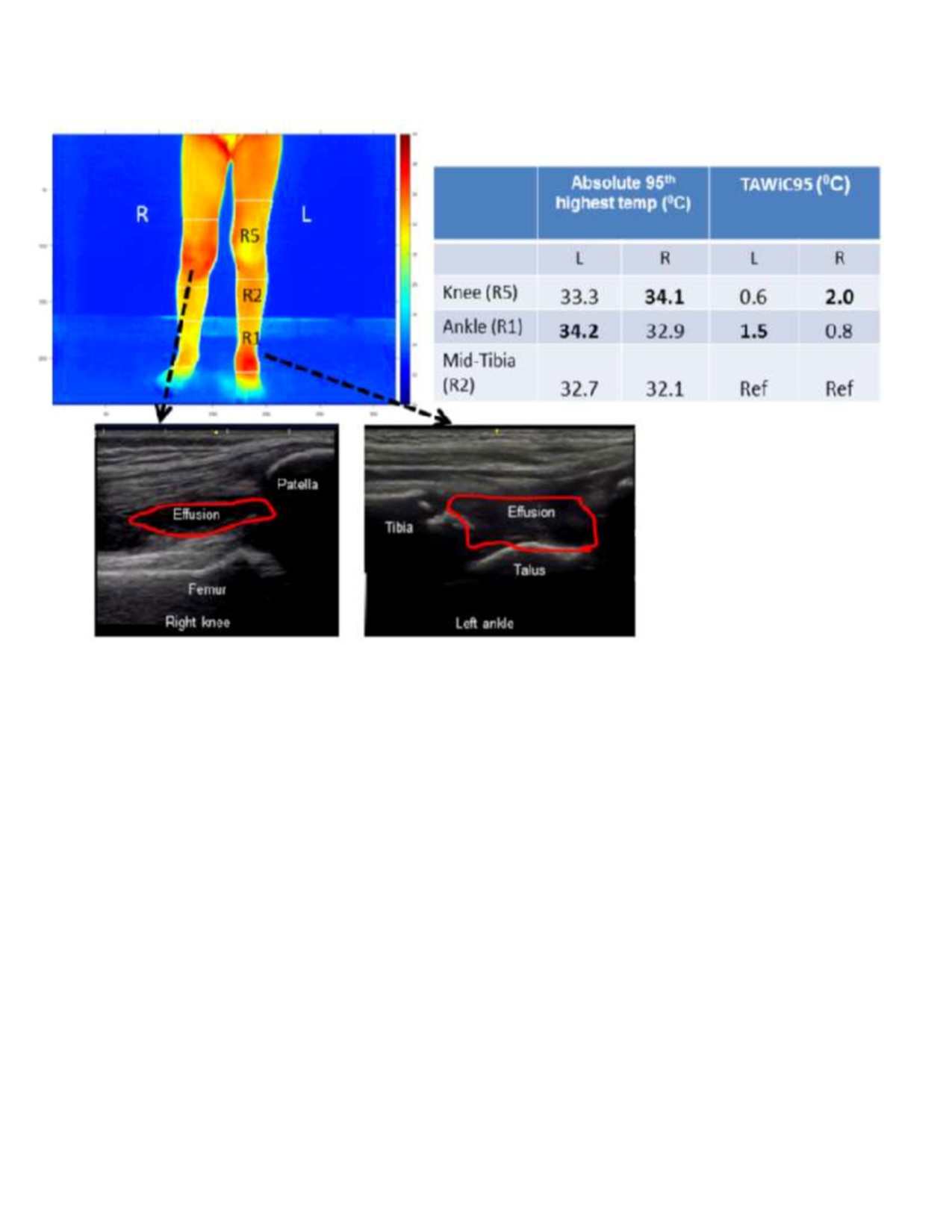
Results: Fifty-one children in the arthritis group and 48 healthy children enrolled had analyzable thermal images and were included in the analysis. Demographic and clinical characteristics are summarized in Table 1. Thermal and ultrasound images and results are shown for one case in Figure 1. Median and 95th percentile absolute temperatures as well as TAWiCmedian and TAWiC95 of knees and ankles are reported in Table 2. For both knee and ankle joints, the p-values and AUC values for distinguishing inflamed from non-inflamed joints are considerably better for TAWiC95 than for absolute temperature, and somewhat better than for TAWiCmedian. AUC for knee TAWiC95 is similar for anterior, lateral and medial views (.85, .83 and .84, respectively) but is lower for posterior view (.60). For ankle joint, only anterior view was analyzable with our algorithm, giving AUC for TAWiC95 of .70. Using anterior view TAWiC95, a cutoff of 0.60 oC for knee gives sensitivity of 0.71 and specificity of 0.91, while a cutoff of 0.13 oC gives sensitivity of 0.72 and specificity of 0.60.
Conclusion: Children with active arthritis/tenosynovitis in knees or ankles exhibited higher temperature after same-limb calibration than healthy/unaffected joints. This standardized approach shows potential to increase utility of infrared thermal imaging for screening JIA, warranting further investigation.
To cite this abstract in AMA style:
Zhao Y, Iyer R, Thapa M, Biswas D, Cain K, Partridge S, Wallace C. Novel Algorithm to Increase Sensitivity of Detecting Active Arthritis in Children Through Infrared Thermal Imaging [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/novel-algorithm-to-increase-sensitivity-of-detecting-active-arthritis-in-children-through-infrared-thermal-imaging/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/novel-algorithm-to-increase-sensitivity-of-detecting-active-arthritis-in-children-through-infrared-thermal-imaging/