Session Information
Date: Saturday, November 16, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The increasing use of imaging techniques, particularly 18F-FDG PET-CT, has significantly expanded our understanding of giant cell arteritis (GCA). Our aim was to examine the frequency and types of non-classical organ involvement in patients with GCA.
Methods: Retrospective study of 148 patients with proven GCA diagnosed between 2005 and 2023. 18F-FDG PET-CT was performed in 142 cases. A causal link to GCA was established when manifestations were identified at diagnosis or within 6 weeks after initiating glucocorticoid treatment
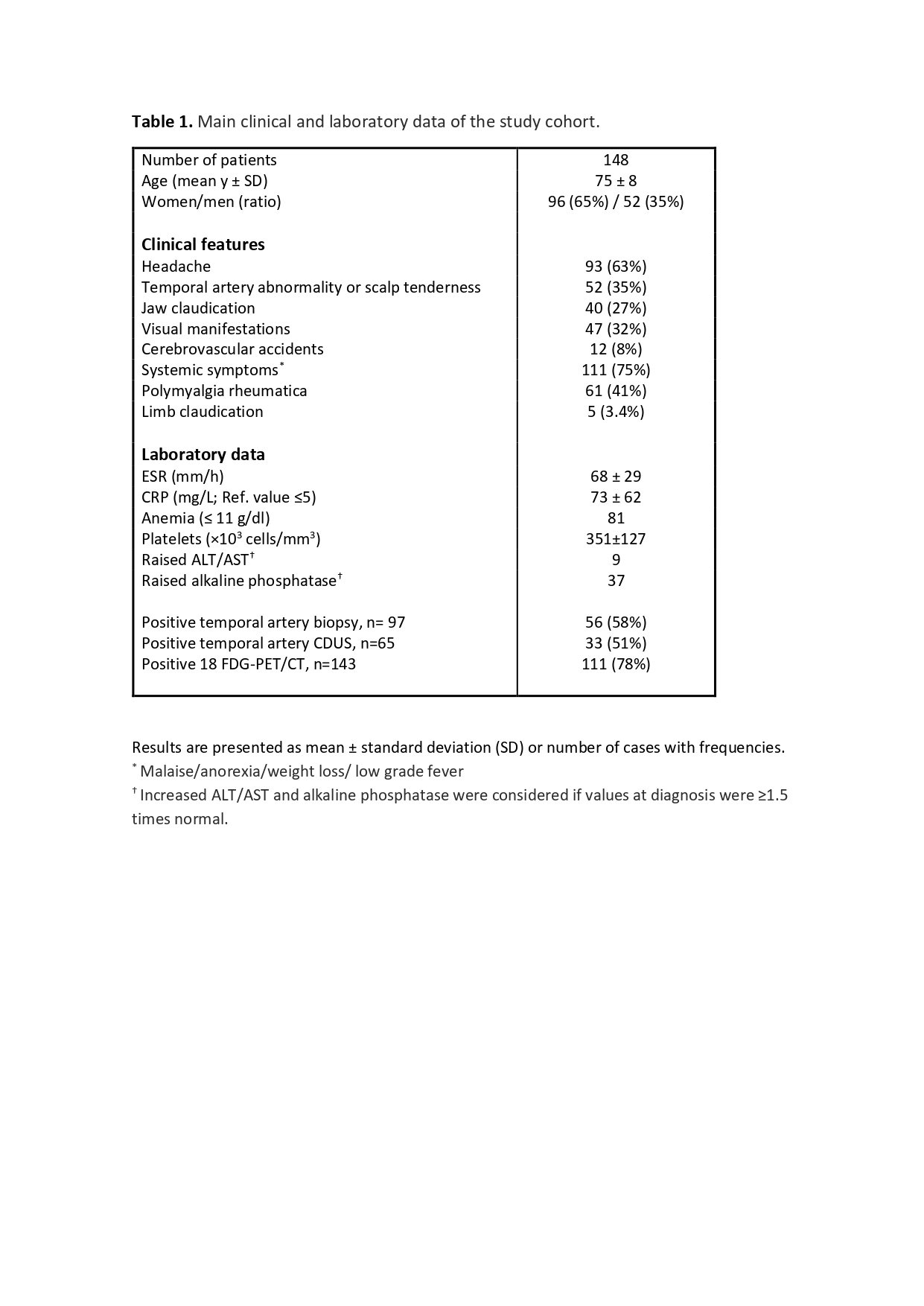
Results: The main clinical features and laboratory data of GCA patients are summarized in Table 1. Among the studied group, 31.1% (46/148) exhibited one or more non-classical complications previously described in the literature. The findings included:
– Cardiac involvement in 8.1% (12/148), with 1 case of ischemic heart disease and 11 (7.4%) of pericardial disease. Clinical pericarditis was diagnosed in 5 patients (3.3%), with 2 having pure pericarditis and 3 with pleuropericarditis. Aortitis was concurrently detected on PET-CT in these 5 patients, with 2 having thoracic aortic aneurysm. Pericardial effusion was observed in another 6 patients, 4 of whom also had pleural effusion. These findings, confirmed by echocardiograms, were not linked to conditions like cardiac insufficiency or hypoalbuminemia.
– Respiratory symptoms in 14.8% (22/148), including 5 patients with odynophagia (3.3%), dry cough in 3 (2%), pleural disease in 11 (7.4%), and ILD in 2 (1.3%). Four patients (2.7%) presented with pulmonary nodules at diagnosis. These nodules completely resolved following corticosteroid therapy, suggesting an inflammatory origin. PET-CT scans showed pulmonary artery involvement in 2 patients (1.3%), both with concurrent PMR findings.
– Neurological involvement, excluding strokes, was present in 2.7% of cases (4/148). These included 2 cases of peripheral neuropathy (sural nerve biopsy showing demyelinating neuropathy and axonal degeneration), 1 case of epilepsy, and 1 case of acute spinal cord infarction (with negative anti-phospholipid antibodies).
– Renal involvement: vasculitis of the renal arteries on PET-CT was observed in 3.4% of patients (5/148).
– Secondary amyloidosis in 1.3% (2/148)
– Gastrointestinal involvement in 6.1% (9/148), including 7 cases of vasculitis of the mesenteric artery and/or celiac trunk on PET-CT, 1 case of mesenteric panniculitis, and 1 case of severe cholestatic hepatitis.
– Salivary gland involvement (parotid and/or submandibular) was detected via PET-CT in 5.4% (8/148).
Other uncommon manifestations include scalp, tongue, or lip involvement/necrosis in 2.7% (4/148), and cases of seronegative polyarthritis and remitting distal extremity swelling with pitting edema in 4% (6/148)
Conclusion: GCA typically presents with classic cranial ischemic manifestations, fever, constitutional symptoms, and clinical features related to extracranial large-vessel involvement. However, there is an increasing awareness of the occurrence of uncommon or exceptional complications in a significant proportion of patients, which could be the presenting symptoms of GCA. These should be considered in the evaluation and follow-up of patients.
To cite this abstract in AMA style:
Narvaez-García J, Vidal p, Maymó P, Palacios J, Aguilar Coll M, Roig Kim M, De Daniel L, Nolla J. Non-classical Organ Involvement in Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/non-classical-organ-involvement-in-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/non-classical-organ-involvement-in-giant-cell-arteritis/