Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatic diseases (RDs) require consistent management with disease-modifying antirheumatic drugs (DMARDs) and regular medical follow-up. However, non-adherence to medication and unattended appointments are common challenges in rheumatology practice, affecting treatment outcomes and healthcare resources. The COVID-19 pandemic has exacerbated these challenges, altering patient behavior and access to healthcare services. Understanding the reasons behind non-adherence and unattended appointments, both before and after the pandemic, is crucial for developing effective strategies to improve patient care and treatment outcomes in rheumatology clinics.
Methods: An observational and cross-sectional study was conducted. We included patients ≥18 years old diagnosed with RD who attended both initial and follow-up assessments at our rheumatology clinic from May to September 2023 and agreed to participate. Patients who missed appointments were contacted to determine reasons for non-attendance. A questionnaire evaluated DMARD usage, adherence, and reasons for non-adherence. Adherence was categorized based on intake frequency: Good ( >75% of the time, >21 days), regular (50-74%, 15-21 days), poor (25-49%, 8-14 days), and null (< 25%, 7 days or less). To compare adherence during the COVID-19 pandemic, data from rheumatology patients in 2021-2022 were used.
Results: Of 4,289 scheduled patients, 2,078 (48.44%) did not attend appointments. Of these, 354 missed their first appointment and 1,724 missed follow-ups. During this period, 78 patients were hospitalized, with 73% attending follow-ups, 23% not attending, and 4% deceased. Economic factors were the primary cause of non-attendance (70%), followed by transportation (14%), forgetting (9%), and personal reasons (2%).
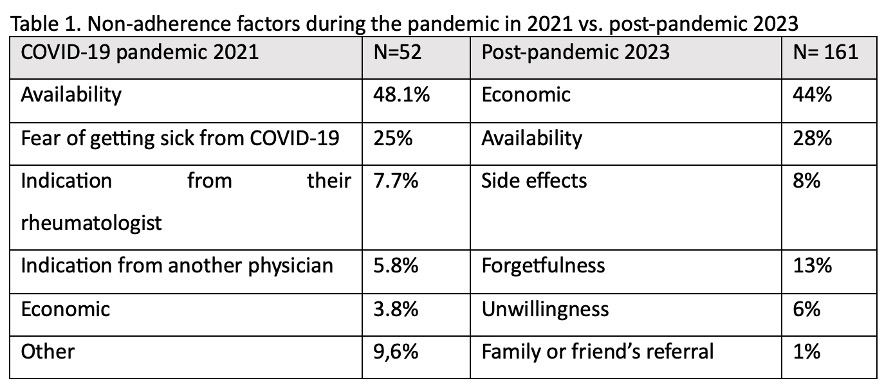
Of 161 patients evaluated for DMARD adherence, 135 (83.8%) had good adherence. Hydroxychloroquine was used by 34% of patients, followed by methotrexate (29%), prednisone (16%), leflunomide (8%), mycophenolate mofetil (8%), azathioprine (3%), and sulfasalazine (2%). Reasons for non-adherence in 2021 and 2023 are shown in Table 1.
Conclusion: Non-attendance and DMARD adherence depend on economic and social circumstances. During the COVID-19 pandemic, fear of infection and limited availability of medications were significant factors contributing to non-adherence. Post-pandemic, economic factors continued to be the primary barrier, but concerns about side effects and forgetting to take medications became more common.
To cite this abstract in AMA style:
Salcedo-Soto D, Bardan-Inchaustegui A, Gamez-Siller P, Lara Mendez D, Flores-Alvarado D, Esquivel-Valerio J, Cardenas-de la Garza J, Galarza-Delgado D. Non-Adherence and Missed Appointments in Rheumatology: Pre and Post COVID-19 Pandemic Impact [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/non-adherence-and-missed-appointments-in-rheumatology-pre-and-post-covid-19-pandemic-impact/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/non-adherence-and-missed-appointments-in-rheumatology-pre-and-post-covid-19-pandemic-impact/