Session Information
Date: Monday, November 8, 2021
Title: Spondyloarthritis Including PsA – Treatment Poster II: Psoriatic Arthritis I (1329–1363)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Physical activity is recommended for patients with psoriatic arthritis (PsA) especially due to the high prevalence of overweight/obesity, and the risk of comorbidities such as CVD and metabolic syndrome. Further, physical exercise may be beneficial regarding disease activity in patients with arthritis. However, in PsA there is a potential risk of increased disease activity including worsening of enthesitis after physical exercise due to mechanical strain.
The primary aim of this study was to measure the effect of high intensity interval training (HIIT) on bone marrow edema (BME) in MRI of the sacroiliac joints (SIJ) and spine as an objective measure of inflammation. Secondly, we aimed to observe whether there was an association between BME and disease activity markers at baseline.
Methods: 41 PsA patients satisfying CASPAR criteria were recruited from clinics to a randomized clinical trial. The intervention group (N=21) performed HIIT, defined as 4 times 4 minutes training at 85-95% of maximum heart rate on a stationary bicycle 2-3 times a week for 11 weeks. The control group (N=20) was instructed not to change their pre-study physical exercise habits during the study. Patients underwent MRI of the SIJ and spine at baseline, and, at average 13 (range: 8 – 26) days after completion of the intervention. MRI was scored for BME according to the Spondylarthritis Research Consortium of Canada (SPARCC). The minimal important change is 2,5 and 5 in SPARCC BME score for SIJ and spine, respectively. Logistic regression analysis was performed to calculate the odds ratio (OR) with 95% CI for worsening in SPARCC-BME for both SIJ and spine between HIIT and control groups. Disease activity markers like HS-CRP, Dapsa68, Pain, ASDAS-CRP and SPARCC enthesitis index assessed at baseline were compared with SPARCC BME scores for SIJ and spine using linear regression and Mann-Whitney test.
Results: The included patients had a low to moderate disease activity measured by Dapsa68 and ASDAS-CRP (table 1). There was no difference in change of SPARCC-BME in SIJ and spine between the two groups with an OR of 0.56 (95 % CI 0.05 to 6.81) and 1.19 (95 % CI 0.07 to 20.54) for SIJ and spine, respectively, for worsening comparing the HIIT with the control group. At baseline, there was an inverse association between SPARCC enthesitis index and SPARCC-BME of SIJ with a mean difference of -2.34 (95% CI -4.53 to -0.15). The results were confirmed by a Mann-Whitney test (p-value 0.02). There was no association between other disease activity markers and SPARCC-BME of SIJ and spine at baseline.
Conclusion: The risk of increased BME in SIJ and spine as an objective marker of inflammation after 11 weeks of HIIT was not higher in the HIIT group compared to controls in a cohort of PsA patients with low to moderate disease activity. Of interest, the degree of baseline BME in SIJ was inversely associated with the subjectively measured burden of enthesitis. The results support that physical exercise does not cause objective signs of increased disease activity in PsA.
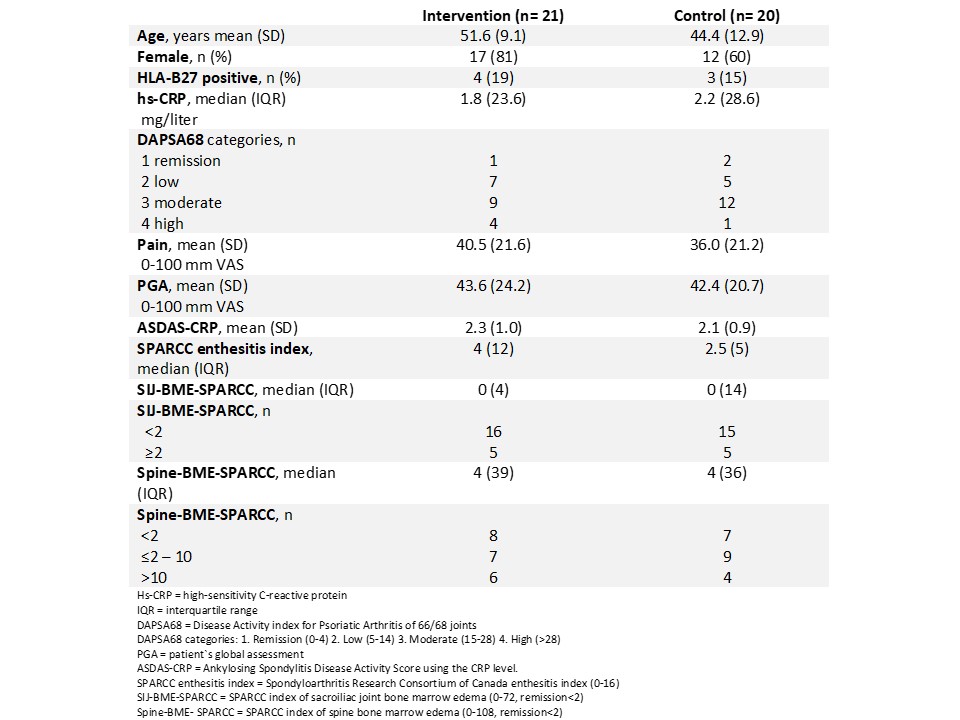 Table 1 Baseline characteristics of the patients with psoriatic arthritis in the intervention and control groups
Table 1 Baseline characteristics of the patients with psoriatic arthritis in the intervention and control groups
To cite this abstract in AMA style:
Thomsen R, Nilsen T, Hoff M, Haugeberg G, Kavanaugh A. No Change in Bone Marrow Edema of the Sacroiliac Joints and Spine After High Intensity Interval Training in PsA [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/no-change-in-bone-marrow-edema-of-the-sacroiliac-joints-and-spine-after-high-intensity-interval-training-in-psa/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/no-change-in-bone-marrow-edema-of-the-sacroiliac-joints-and-spine-after-high-intensity-interval-training-in-psa/
