Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Vertebral osteomyelitis (VO) can be associated with neurological complications. We showed in a previous study that they occurred in 40% of patients with VO. Spine immobilization is recommended to prevent those complications but with poor evidence from the literature.
The aim of our study was to describe the practice of spine immobilization in a large multicentered cohort of patients with VO, and to evaluate the association between immobilization and neurological complications.
Methods: We prospectively recruited patients with VO from 2016 and 2019 in 11 centers. We included adults patients with VO confirmed by imaging and identification of causative agent or a good response to antibiotic therapy if all samples were sterile. We collected clinical, microbiologic, imaging and therapeutic characteristics at admission and during follow up, at 3 and 6 months. Characteristics of the type and duration of immobilization were especially recorded.
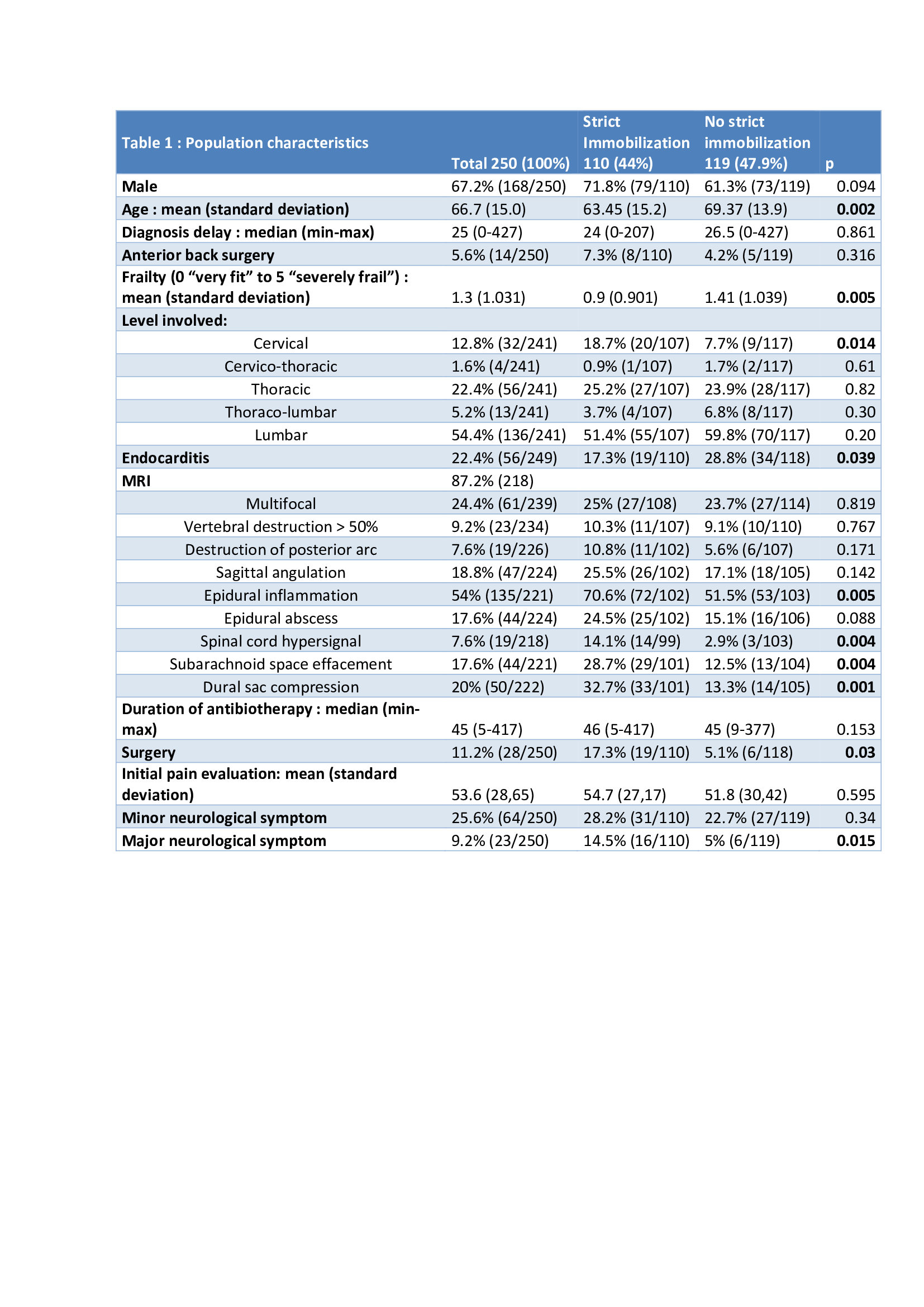
Results: 250 patients were included. Mean age was 66.7 +/- 15 years old, mostly men (67.2%, n=168). Median duration of pain before diagnosis was 25 (0-427) days. Lumbo-sacral level was the most frequently involved (54.4%), cervical level was involved in 12.8% of cases. Staphylococcus aureus was the most frequent pathogen (33.6%).
At diagnosis, 25.6% patients (n=64) had minor neurological symptoms (radicular pain, reflex abolition, sensitive loss) and 9.2% (n=23) major neurological complications (motor weakness or sphincter dysfunction). During follow up, new minor neurological complications occurred in 9.2% (n=23) of patients, and major ones in 6.8% of patients (n=17) medianly 11 (1 to 45) days.
Median duration of antibiotherapy was 45 (5-417) days, 11.2% of patients (n=28) underwent surgery.
Immobilization was prescribed in 69.2% (n=173) of cases, 94.2% (n=162) were rigid bracing. However a strict immobilization (defined by a rigid brace for at least 6 weeks) was prescribed for only 44% of the patients (n=110). In multivariate analysis, factors significantly associated with strict immobilization were: Centre (p=0.035), younger age (p=0.005), dural sac compression (p=0.005) and major neurological signs at diagnosis (p=0.036). Vertebral destruction or epidural abscesses were not associated with strict immobilization. Lumbar localization was not less strictly immobilized.
There was no significant difference in the apparition of new minor neurological complications between strictly immobilized patients and others (10.9% (n=12) and 5.9% (n=7) respectively; log Rank = 0.315). Same results were found for new major complications (4.5% (n=5) and 6.7% (n=8) respectively; log Rank = 0.913).
Duration of immobilization prescription was not associated with apparition of severe complications.
In patients without prescription of any rigid bracing, subarachnoid space effacement was significantly associated with apparition of major neurological complications in multivariate analysis (p=0.016).
Conclusion: Only 44% of the patients were strictly immobilized in our cohort. We did not observe significant differences in terms of neurological complications between strictly immobilized patients and others.
To cite this abstract in AMA style:
Le Pluart A, Guillaume C, Darrieutort C, Grégoire C, Sophie G, Ottaviani S, Nocturne G, Oriane M, Marion C, Emmanuel H, Denis M, Le Goff B, Bart G. “No Benefit from a Strict Immobilization in Vertebral Osteomyelitis” Vertebral Immobilization and Neurological Complication in Acute Pyogenic Vertebral Osteomyelitis: SPONDIMMO, a Prospective Cohort of 250 Patients [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/no-benefit-from-a-strict-immobilization-in-vertebral-osteomyelitis-vertebral-immobilization-and-neurological-complication-in-acute-pyogenic-vertebral-osteomyelitis-spondimmo-a-pros/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/no-benefit-from-a-strict-immobilization-in-vertebral-osteomyelitis-vertebral-immobilization-and-neurological-complication-in-acute-pyogenic-vertebral-osteomyelitis-spondimmo-a-pros/