Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Takayasu arteritis (TA) is a large vessel vasculitis of unknown pathogenesis. The current serological and radiological parameters used to assess disease activity are not highly specific and there is a need for a relevant biomarker. In our previous study [1], NMR based serum metabolomics had revealed distinctive metabolic signatures in patients with TA compared to age/sex matched healthy controls and SLE [2]. In this study we investigate whether these distinctive metabolites correlate with disease activity.
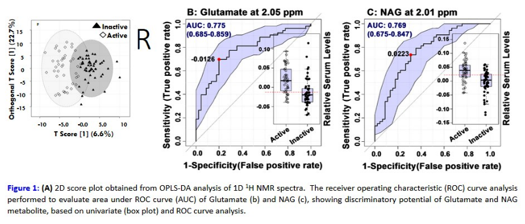
Methods: Patients with TA fulfilling ACR criteria were assessed for disease activity using ITAS A (ESR), with a score of ³4, considered as active. The serum metabolic profiles of active and inactive TA patients obtained with an 800 MHZ NMR spectrometer were compared using multivariate orthogonal partial least-squares discriminant analysis (OPLS-DA) to identify metabolites that related to disease activity [based on PLS-DA VIP(variable importance on projection) score >1.5 and permutation test, p-value < 0.01].
Results: 98 patients were categorized into active (45) and inactive (53) groups – median age 27 years in both groups and female to male ratio 3.5:1 and 4.9:1 respectively. The majority had class V disease. Mean duration of illness was 8.8 ± 13.2 years in active TA and 5.2 ± 5.6 years in inactive TA group. An exquisite separation in OPLS-DA score plot showed metabolic differences between active and inactive TA patients (Fig. 1A). The key metabolites with highest discriminatory potential (VIP score > 1.5) which were elevated in active TA were glutamate, N-acetyl glycoprotein (NAG), glucose, phosphoglyceride, glycerol, leucine whereas lactate, choline, low/very-low density lipoproteins (LDL/VLDL) were decreased. Receiver operating characteristic (ROC) curve analysis revealed glutamate and NAG had the highest potential to discriminate active from inactive TA (area under the curve 0.775 and 0.769 respectively (p-value<0.0001) (Fig. 1B, 1C). The spectra did not correlate with current therapy but did alter when disease activity changed on follow-up.
Conclusion: This large cohort of patients revealed metabolic profiles discriminating between clinically active and inactive TA patients. It suggests glutamate and NAG have strong potential as biomarkers for disease activity in TA and may serve as a guide to therapy. We are now working to further validate these results in longitudinal studies.
References
1. Guleria A, Misra DP, Rawat A, Dubey D, Khetrapal CL, Bacon PA, Misra R, and Kumar D, NMR based serum metabolomics discriminates Takayasu Arteritis from Healthy Individuals: A proof of principle study, Journal of Proteome Research 2015 :14;3372-3381.
2. Misra R, Guleria A, Misra DP et al NMR-Based Metabolomics Provides New Insights into the Inflammatory Processes in Takayasu Arteritis [abstract]. Arthritis Rheumatol. 2015; 67
To cite this abstract in AMA style:
Misra R, Jain A, Kumar D, Misra DP, Guleria A, Kumar S, Rawat A, Chaurasia S, Kumar U, Zanwar A, Dubey D, Goel R, Danda D, Bacon P. NMR-Based Serum Metabolomics of Patients with Takayasu Arteritis (TA) and Relationship with Disease Activity [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/nmr-based-serum-metabolomics-of-patients-with-takayasu-arteritis-ta-and-relationship-with-disease-activity/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nmr-based-serum-metabolomics-of-patients-with-takayasu-arteritis-ta-and-relationship-with-disease-activity/