Session Information
Date: Sunday, October 26, 2025
Title: (0671–0710) Systemic Sclerosis & Related Disorders – Clinical Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Elevated neutrophil-to-lymphocyte ratio (NLR) in systemic sclerosis (SSc) has been demonstrated to predict worsening skin and lung involvement, and a cutoff of 2.95 was shown to be related to a decreased 5-year survival in a recent pilot study. The aim of this study was to further define a cutoff of baseline NLR that predicts poor outcome of SSc and to explore longitudinal variations of NLR with respect to disease onset in a large healthcare database.
Methods: Adult SSc patients from the Maccabi healthcare services (MHS) database,a 2.7-million-member, state-mandated, health provider in Israel, between 2003 and 2023 were included. Identification algorithm included an ICD 9 diagnosis of “systemic sclerosis” or “scleroderma” by a rheumatologist or at hospital discharge or a diagnosis in the presence of at least one high titer autoantibody (ANA or SCL-70 or anticentromere or anti RNA POLIII ).
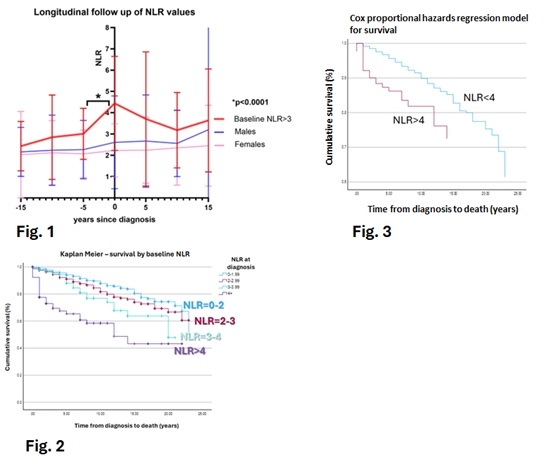
Results: Overall, 1752 SSc patients fulfilled the inclusion criteria over the study period. In 2023 the estimated prevalence of SSc in Israel was 735 per million. 241 patients were excluded because of steroid use. Thus, baseline study cohort included 1511 patients of whom 1232 had NLR values at baseline (Table1). The mean NLR at diagnosis was 2.21±1.36, including 110 (9%) with value between 3-4 and 81 (6.5%) above 4. At diagnosis, NLR was significantly higher in men, in patients with pulmonary fibrosis (n=245, 16%), pulmonary hypertension (n=233, 15%), and with MMF treatment (n=139, 9%). In patients with a high baseline NLR >3 (n=191, NLR 4.4±2.21), NLR showed a statistically significant increase at onset when compared to values measured 1, 5, 10, and 15 years prior to diagnosis (Figure 1). Thirty six percent of these patients had specific antibodies up to 15 years before diagnosis. NLR did not change over time or with therapy over 15 years of follow-up after diagnosis (Figure 1). During 20 years of follow-up, 360 patients (20%) died. Each 1-point increase in baseline NLR was linked to higher 5- and 10-year mortality rates, as demonstrated by the Kaplan-Meier curve (figure2). The highest mortality rates were observed in NLR >4, reaching 25% at 5 years and 31% at 10 years (p < 0.001), (Figure 2). A Cox regression model that included covariables (age, sex, pulmonary fibrosis, pulmonary hypertension) found in patients with NLR above 4 had a hazard ratio of 2.83 (-2 log-likelihood chi-square = 277.3, p < 0.001) for time to death (Figure 3).
Conclusion: This extensive cohort study confirms that a high baseline NLR is predictive of 5- and 10-year mortality, with a refined threshold of NLR greater than 4. Male sex, pulmonary fibrosis and pulmonary hypertension were key risk factors for high baseline NLR and predicted mortality. Notably, elevated NLR was already present at disease onset—even when autoantibodies appeared earlier and remained persistently high for over 15 years, unaffected by treatment. NLR was not correlated with CRP and therefore is not a surrogate marker for inflammation. These findings support the use of NLR as a simple, accessible biomarker to identify high-risk SSc patients who may benefit from closer monitoring and more intensive therapeutic strategies.
.jpg) Table 1 – demographic and Clinical and characteristics
Table 1 – demographic and Clinical and characteristics
To cite this abstract in AMA style:
Keret S, Yaari S, Slobodin g, Rimar d. Neutrophil-to-Lymphocyte Ratio as a biomarker for disease onset and a predictor for mortality in Systemic Sclerosis – real-world data from a large healthcare provider in Israel. [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/neutrophil-to-lymphocyte-ratio-as-a-biomarker-for-disease-onset-and-a-predictor-for-mortality-in-systemic-sclerosis-real-world-data-from-a-large-healthcare-provider-in-israel/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neutrophil-to-lymphocyte-ratio-as-a-biomarker-for-disease-onset-and-a-predictor-for-mortality-in-systemic-sclerosis-real-world-data-from-a-large-healthcare-provider-in-israel/