Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Neuropsychiatric systemic lupus erythematosus (NPSLE) remains a challenging entity to diagnose and treat. The clinical heterogeneity of NPSLE coupled with the difficulty with attribution of neuropsychiatric symptoms to SLE contribute to the challenges in diagnosis. Furthermore, recommendations for diagnosis and treatment may be limited in their applicability to childhood-onset SLE (cSLE), as there are limited diagnostic tools and treatments and current evidence is largely extrapolated from adult studies. The objective of this scoping review is to review the current literature on NPSLE in cSLE (cNPSLE), grade the level of evidence and identify knowledge gaps in the scope of clinical manifestations, diagnosis, predictors, treatment, and outcomes of cNPSLE.
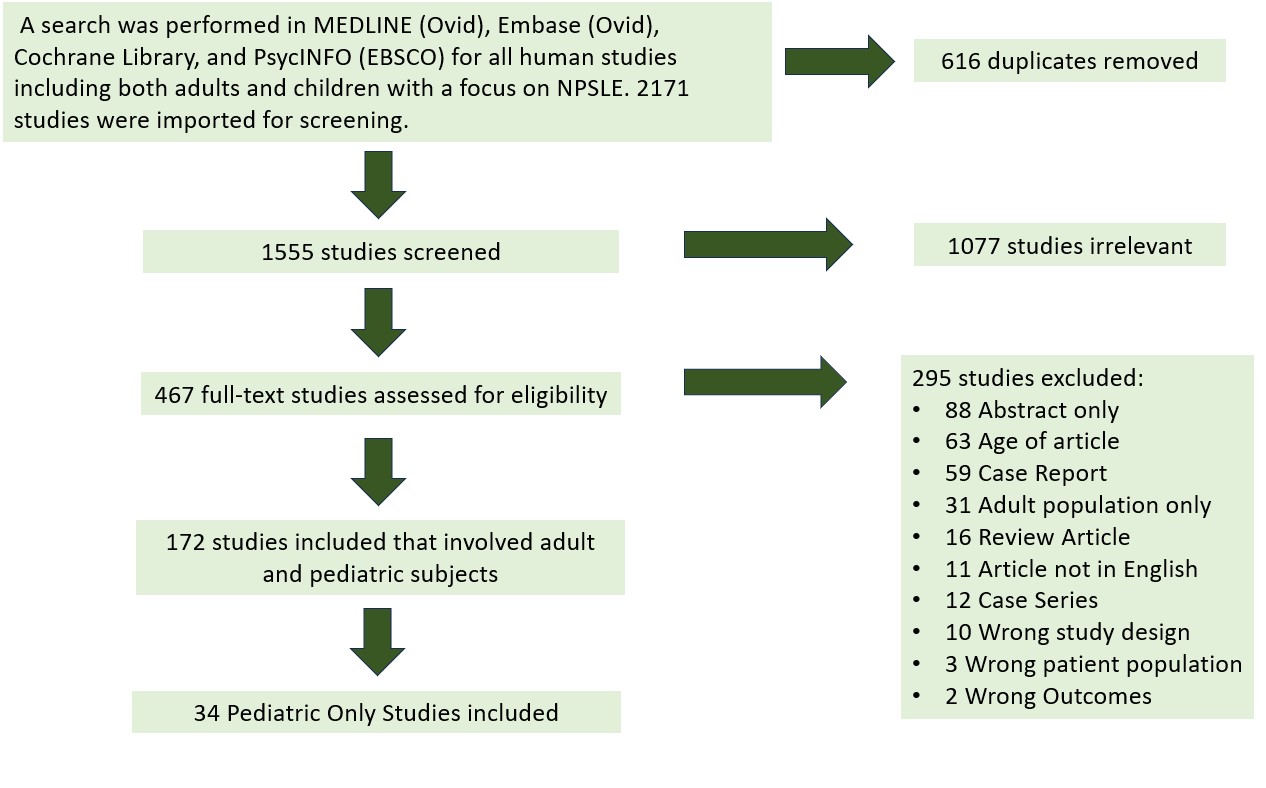
Methods: An exhaustive search was performed in MEDLINE, Embase, Cochrane, and PsycINFO. Articles were screened in Covidence. We included articles of systematic reviews, cohort, case-control and cross-sectional studies published between 2000 and 2022, studies involving children aged 18 years or younger diagnosed with NPSLE, and only original manuscripts available in English. Five reviewers performed abstract and full-text screening. Eight reviewers performed data extraction. Full text extraction was performed by two reviewers and any conflicts were resolved by a third reviewer. Thirty-four articles met our study eligibility criteria (Figure 1). The certainty of the evidence was assessed using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) methodology.
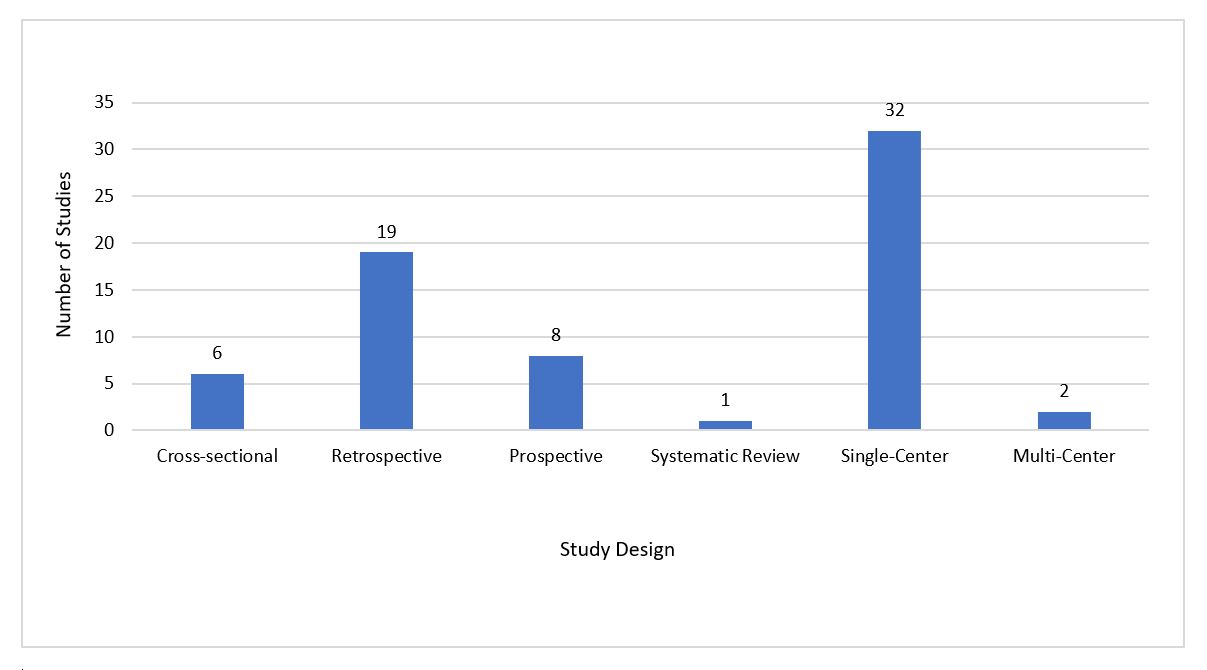
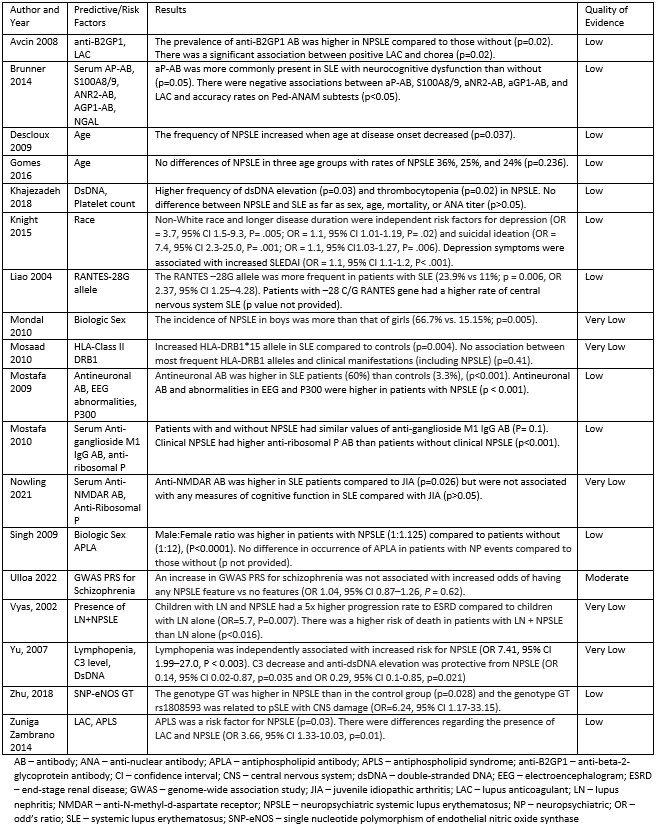
Results: Article characteristics are shown in Figure 2. The prevalence of cNPSLE ranged from 17% to 95%. The mean age in years was 13.7 +/- 4.6. The most common clinical manifestations were cognitive dysfunction (8-100%), headaches (13-85%), and seizures (19-84%). However, some studies did not classify mood disorders or headaches as NPSLE manifestations. Predictive factors of cNPSLE are shown in Table 1. Cerebral and cerebellar volume loss and white matter hyperintensities were the most common findings on MRI, though many patients with active cNPSLE had a normal MRI. Ped-ANAM was the only validated screening tool to assess neurocognitive dysfunction in cNPSLE. Only one study focused primarily on treatment for cNPSLE; this was retrospective and focused on psychosis. Complete recovery of NSPLE ranged from 40-86%, and mortality from 5-45%. Causes of death included status epilepticus, cerebrovascular accident, infection, and brainstem encephalitis.
Conclusion: This scoping review addresses significant knowledge gaps about cNPSLE. Most studies were retrospective, single center studies, with low quality of evidence. The wide range in the prevalence and frequency of cNPSLE manifestations is likely due to the lack of consensus in methods for definition and evaluation of cNPSLE. The evidence of treatment for cNPSLE is also sparse. We highlight the need for further prospective, multicenter studies, and consensus regarding approaches to cNPSLE investigation and management. The results of this work also provide the literature background (first phase) in a project to develop a multi-disciplinary, patient-centered prioritized research agenda for cNPSLE.
To cite this abstract in AMA style:
Theisen A, Ogbu E, Beil E, Harry O, Appenzeller S, Kammeyer R, Van der Heijen H, Knight A, Craven H, Rodriguez M. Neuropsychiatric Systemic Lupus Erythematosus in Children: A Scoping Review [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/neuropsychiatric-systemic-lupus-erythematosus-in-children-a-scoping-review/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neuropsychiatric-systemic-lupus-erythematosus-in-children-a-scoping-review/