Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Neuropsychiatric systemic lupus erythematosus (NPSLE) has a significant impact on morbidity associated with SLE. However, the prevalence of NPSLE has been reported variably based on the definition used and ethnicity. Data from prospective cohorts is limited across the world, and no data is available from South Asia. We studied the NPSLE features and their associations at baseline visits in the Indian SLE prospective cohort for research (INSPIRE), a multicentric prospective cohort.
Methods: The INSPIRE database, accessed on May 1, 2024, has enrolled 2503 adults and children with SLE satisfying SLICC classification criteria at their first visit to the hospital. Data regarding demographic, clinical and laboratory features, including NP manifestations, were extracted. Attribution of NPSLE has been done based on physician’s judgement guided by the ACR definitions. The 6 monthly follow-up data included flares (type, organ involved), mortality and new organ involvement.
Besides descriptive statistics multivariable logistic regression was done to look for factors associated with NPSLE. In addition, an association of anti-phospholipid antibodies with stroke was also analysed.
Results: The 2503 patients with SLE had a mean age of 27.7±10.2 years, with 495 having a juvenile-onset disease. The majority were females (2291, 91.1%), with a median disease duration of 10 (4-24) months.
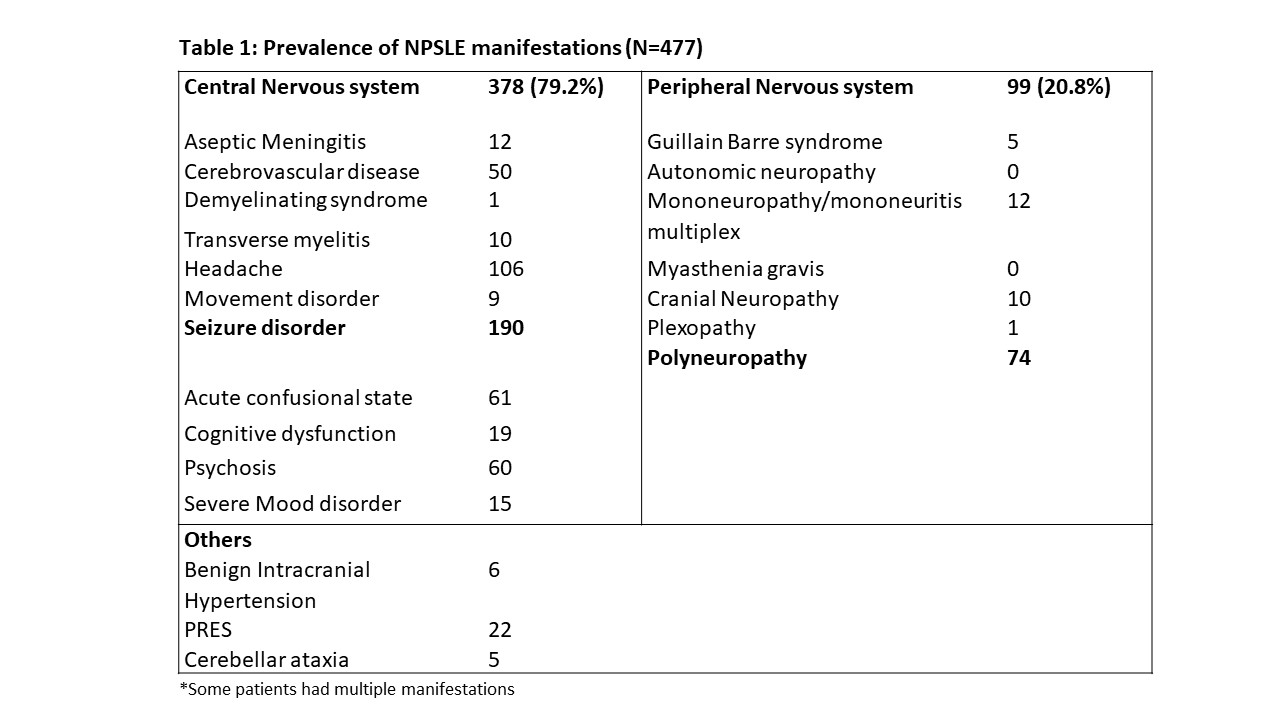
A diagnosis of NPSLE was made in 477 (19%) patients. These patients (89.5% females, mean age:27.4±10.5 years) had a median symptom duration of 10 months, mean SLEDAI of 13.5± 8.5 and mean SLICC Damage Index of 0.13±0.39 at their first presentation. Central nervous system involvement was seen in 79.2%. Among the NPSLE patients, seizures were recorded in 190(39.8%), headache in 106(22.2%) and polyneuropathy in 74(15.5%). Rarer manifestations included catatonia, plexopathy and demyelinating syndrome.(Table 1)
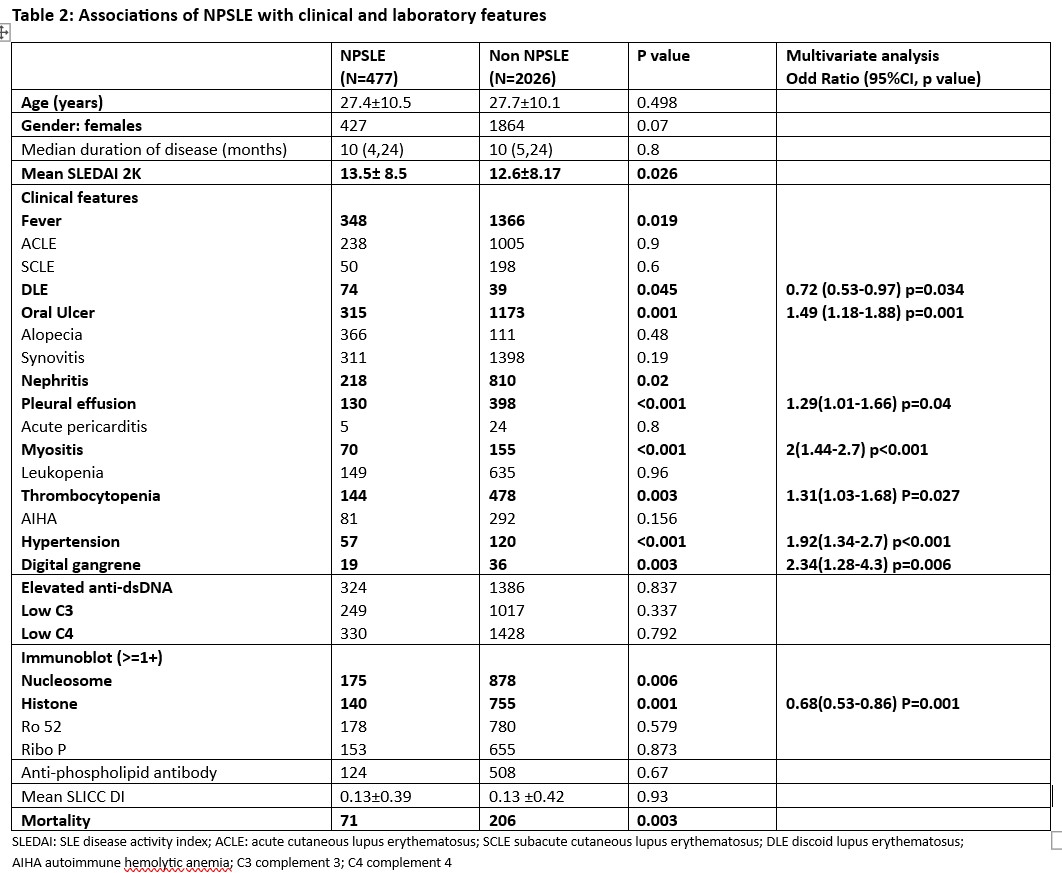
NPSLE patients had higher SLEDAI, higher damage as compared to non-NPSLE patients. Fever, oral ulcer, nephritis, myositis, pleural effusion, thrombocytopenia, gangrene and hypertension were positively associated, while DLE was negatively associated with NPSLE patients as compared to non NPSLE patients. (Table 2)
In addition, the presence of antiphospholipid antibodies was associated with a higher risk of stroke, while hypertension was associated with stroke, acute confusional state and seizure. A higher proportion of gangrene was noted in patients with polyneuropathy and mononeuritis/ mononeuritis multiplex.
During the 2005 patient-year follow-up period so far (NPSLE 931 patient-years), 10 NPSLE flares occurred (all in the first 24 months), and 29 new patients developed NPSLE. Among the 277 deaths, 71 were patients who presented with NPSLE. There were 5 deaths by suicide, of which 2 were in patients with NPSLE. Patients with NPSLE had a higher mortality as compared to those without NPSLE (p=0.003).
Conclusion: About a fifth of patients with SLE have neuropsychiatric manifestations at presentation, and they tend to have higher damage and activity. The recurrence rate is low, and mostly in the first 2 years of follow-up.
To cite this abstract in AMA style:
Kommaraju S, Rajasekhar L, Mathew A, Shobha V, Ghosh P, Kavadichanda C, Lawrence A, Das B, Rathi M, Gupta R, Jain A, Aggarwal A. Neuropsychiatric Manifestations in Indian SLE Inception Cohort for Research: Prevalence, Predictors and Outcomes [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/neuropsychiatric-manifestations-in-indian-sle-inception-cohort-for-research-prevalence-predictors-and-outcomes/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neuropsychiatric-manifestations-in-indian-sle-inception-cohort-for-research-prevalence-predictors-and-outcomes/