Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: In psoriatic arthritis (PsA) peripheral nociceptive pain is characteristic, and is trigger by the activation of the afferent sensory fibers in the inflamed synovial membrane. The greatest ability to respond to pain in the presence of inflammation is physiological, however, pain hypersensitivity may persist after inflammation has resolved and perpetuate itself as chronic pain, a mechanism in which central hypersensitivity is involved. Inflammatory activity indices include subjective variables related to pain perception, so central hypersensitivity can overestimate disease activity. For this reason, identifying possible underlying pain mechanisms can be of great importance in clinical decision-making. Purpose: To relate the presence of neuropathic pain with disease activity and impact, and to analyze the influence of comorbidity on neuropathic pain.
Methods: Cross-sectional study of 246 PsA patients (diagnosed with CASPAR criteria). Patients with fibromyalgia, depression, anxiety or diabetes were excluded. The PAINDETECT questionnaire was used to identify neuropathic pain and to classified patients into 3 groups: a score ≥ 19 indicated a high probability of pain with a neuropathic component, between 18 and 13 was ambiguous and ≤ 12 possibly ruled out this type of pain. Disease activity was measured by DAPSA index, ESR and CRP. The therapeutic objective was the minimal disease activity (MDA) and to assess disease impact PsAID questionnaire was used. Regarding comorbidities anxious and/or depressive habit were assessed using the Hospital Anxiety and Depression Scale (HADS), fatigue (item 2 of PsAID), sleep quality by the Insomnia Severity Index (ISI) and waist-to-hip ratio, apolipoprotein A, apolipoprotein B, lipoprotein A, C-peptide, insulin, insulin resistance (HOMA) and leptin were also measured.
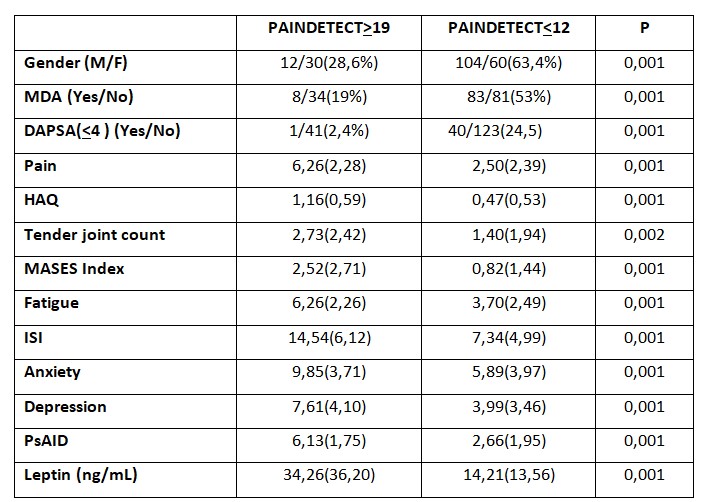
Results: Of the 246 patients 44.7% were female and the mean of age was 53.45 years (SD: 11.00). The average disease duration was 10.3 years (SD: 7.47). 64.6% were taking synthetic DMARDs and 14.6% were receiving biological therapy. 24.8% were in remission by DAPSA and 39.4% achieved MDA. According to the PAINDETECT questionnaire 17.1% of patients had neuropathic pain and 66.7% didn’t. Table 1 shows the significant variables related to neuropathic pain.
In the multivariate analysis composed of gender, ISI, HADS, fatigue, leptin and obesity, the variables that influenced the presence of neuropathic pain were fatigue p < 0.003 (OR: 1.34, 95% CI: 1,10-1.62), sleep quality p < 0.001 (OR: 1.20; 95% CI: 1.10-1.32) and leptin p < 0.008 (OR: 1.03; 95% CI: 1.008-1.052). Nagelkerke's R2 = 0.51.
Conclusion: PsA patients with neuropathic pain have higher probability of not achieving MDA or remission measured by DAPSA. More intense pain, greater number of entheses and tender joints were the main reasons. Therefore, neuropathic pain assessment in our patients may have therapeutic implications. Sleep quality and fatigue influenced the presence of neuropathic pain, and these processes (secondary to central hypersensitivity) were associated to PsA and not to other diseases such as fibromyalgia. As described in animal models, leptin levels could mediate in the presence of chronic pain.
To cite this abstract in AMA style:
Acosta M, Compán O, Pastor S, Manzano Canabal G, Gomez-Lechon Quiros L, Hidalgo Calleja C, Martinez Gonzalez O, Turrión A, Del Pino-Montes J, Montilla Morales C. Neuropathic Pain Relationship with Comorbidity in Psoriatic Arthritis Patients and Its Influence on Disease Activity [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/neuropathic-pain-relationship-with-comorbidity-in-psoriatic-arthritis-patients-and-its-influence-on-disease-activity/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neuropathic-pain-relationship-with-comorbidity-in-psoriatic-arthritis-patients-and-its-influence-on-disease-activity/