Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: To investigate whether neuropathic pain is present in patients with inflammatory hand OA, to investigate characteristics of those patients and the impact of neuropathic pain on quality of life (QoL), and whether neuropathic pain is influenced by anti-inflammatory treatment.
Methods: Data from a randomized, double-blind, placebo-controlled trial in which 92 patients with hand OA fulfilling ACR criteria were treated with prednisolone, has been analysed. Patients had signs of synovial inflammation, a VAS finger pain of ≥30 and showed flaring ≥20 upon NSAID washout. The primary endpoint of this trial was VAS finger pain (0-100) at week 6.
Neuropathic pain was measured at baseline and after treatment by the painDETECT questionnaire, consisting of questions on pain quality, pain intensity over time and radiating pain. Total score: -1 to 38. Scores< 12 unlikely, scores 13-18 undetermined, scores >18 likely neuropathic pain. QoL was measured with physical component scale (PCS) of Short-Form 36 (SF36; 0-100), comorbidities with the Self-administered Comorbidities Questionnaire (SCQ; 0-45); radiographic severity with Kellgren-Lawrence (KL) sumscore (0-120). OMERACT-OARSI responder criteria were used to determine response on prednisolone.
Association of patient characteristics with neuropathic pain was analysed with multivariate multinominal logistic regression with painDETECT categories as dependent variable. Association of neuropathic pain with QoL was analysed with multivariate linear regression, adjusted for age, sex, BMI, VAS finger pain, SCQ score and KL sumscore, with PCS as dependent variable. Response of neuropathic pain to prednisolone was analysed with generalised estimating equations. Association of neuropathic pain at baseline with response to treatment were analysed using chi-squared tests.
Results: 91 Patients had complete painDETECT data at baseline (mean 12.8 (SD 5.9)). Of these, 53% had no neuropathic pain, 31% were undetermined and 16% had neuropathic pain. Higher painDETECT scores at baseline were associated with lower age, female sex, less radiographic damage and more comorbidities in multivariate analysis (table 1).
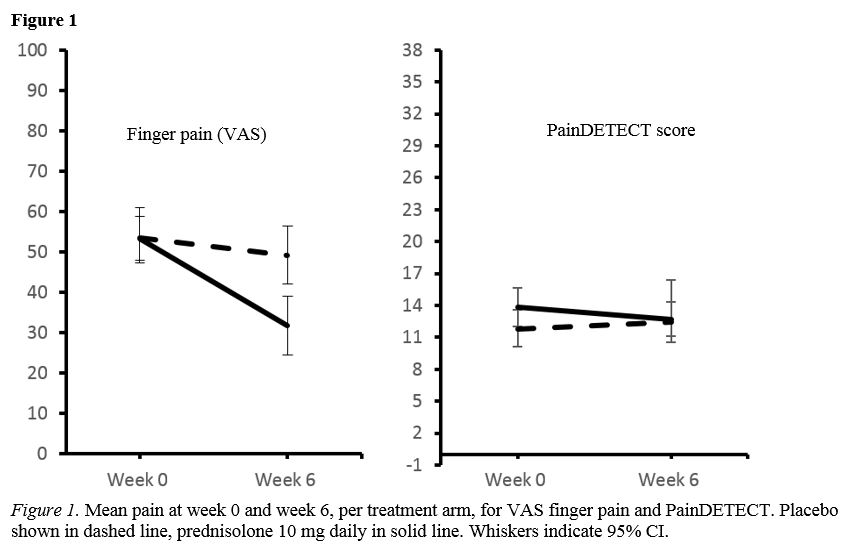
Patients with likely neuropathic pain had a lower QoL ( PCS -6.5 (95%CI -10.4 to -2.6), than those without (painDETECT < 13). Neuropathic pain did not change during the trial in both treatment groups, and there was no difference in painDETECT scores between the groups (between group difference mean -1.7 (95%CI -3.9 to 0.4)). VAS pain improved more in the prednisolone group than in the placebo group (between group difference mean -16.5 (95%CI -26.1 to -6.9)) (figure 1). In this study we could not show an association between the presence of neuropathic pain at baseline and OMERACT-OARSI response to treatment (data not shown).
Conclusion: Patients with inflammatory hand OA and additional neuropathic pain are more often female and have more comorbidities, and report a lower QoL, than those without. Neuropathic pain seems unresponsive to anti-inflammatory therapy. Clinicians should be aware of the presence of neuropathic pain in their patients as these findings might implicate that this kind of pain should be specifically targeted.
To cite this abstract in AMA style:
van der Meulen C, van de Stadt L, Kroon F, Kortekaas M, Boonen A, Böhringer S, Reijnierse M, Rosendaal F, Riyazi N, Starmans M, Turkstra F, Van Zeben J, Allaart C, Kloppenburg M. Neuropathic Pain in Inflammatory Hand Osteoarthritis(OA) Lowers Quality of Life and May Require Another Approach Than Anti-inflammatory Treatment [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/neuropathic-pain-in-inflammatory-hand-osteoarthritisoa-lowers-quality-of-life-and-may-require-another-approach-than-anti-inflammatory-treatment/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neuropathic-pain-in-inflammatory-hand-osteoarthritisoa-lowers-quality-of-life-and-may-require-another-approach-than-anti-inflammatory-treatment/