Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Prosthetic joint complications (PJC) are a major concern after joint replacement surgeries especially in patients with history of inflammatory arthritis. We aimed to compare PJC hospitalizations among patients with and without inflammatory arthritis (IA).
Methods: We utilized the 2016-2020 National Inpatient Sample (NIS) Database to obtain all PJC hospitalizations. These were divided into two groups of with and without IA (Rheumatoid Arthritis, Spondylarthritis, Psoriatic Arthritis or Inflammatory Bowel Disease related arthritis). The two groups were compared for demographics, length of stay, total charges and outcomes using Chi square and Wilcoxon rank-sum tests. We also compared individual PJC in all adult hospitalizations with and without IA.
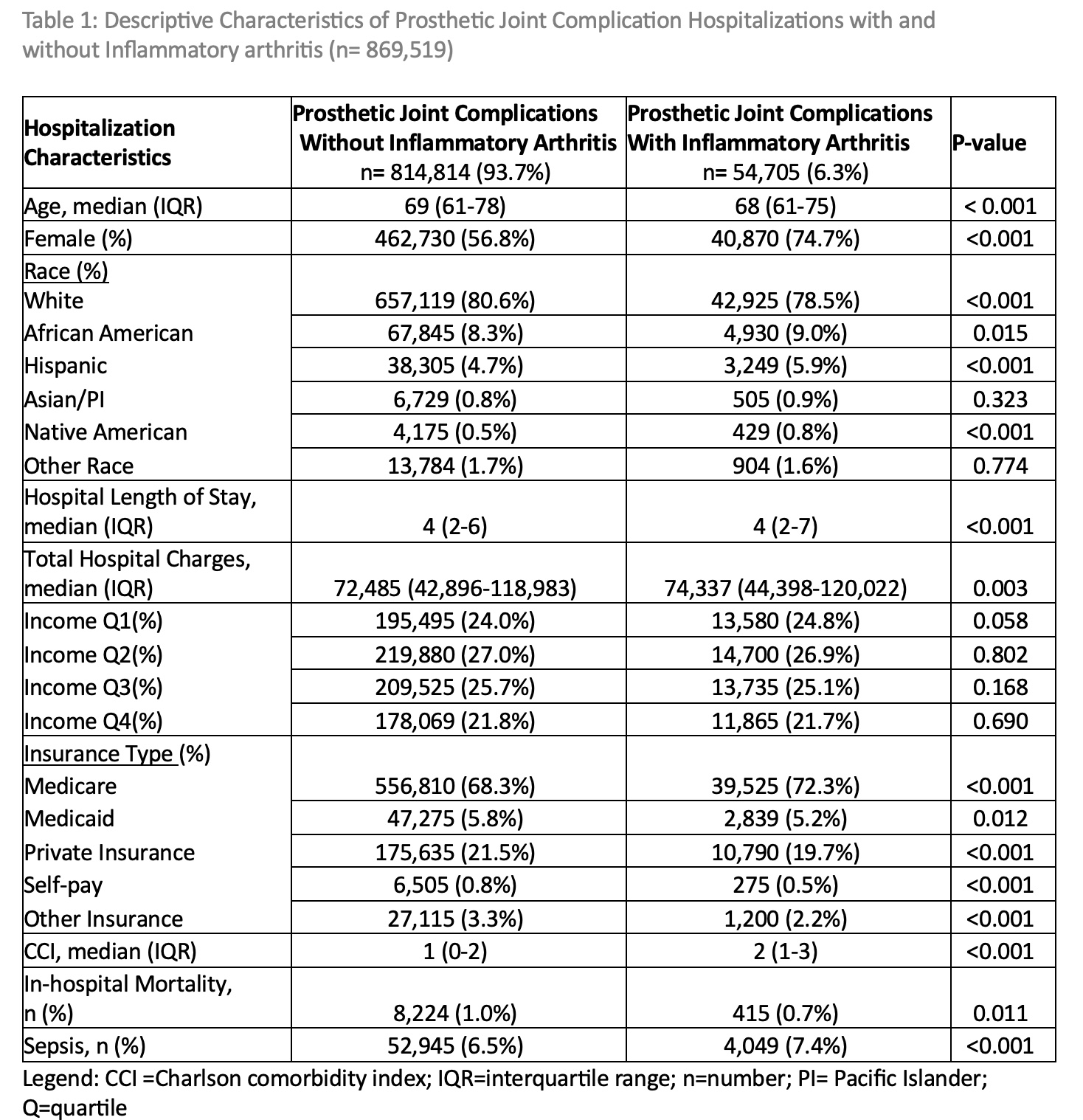
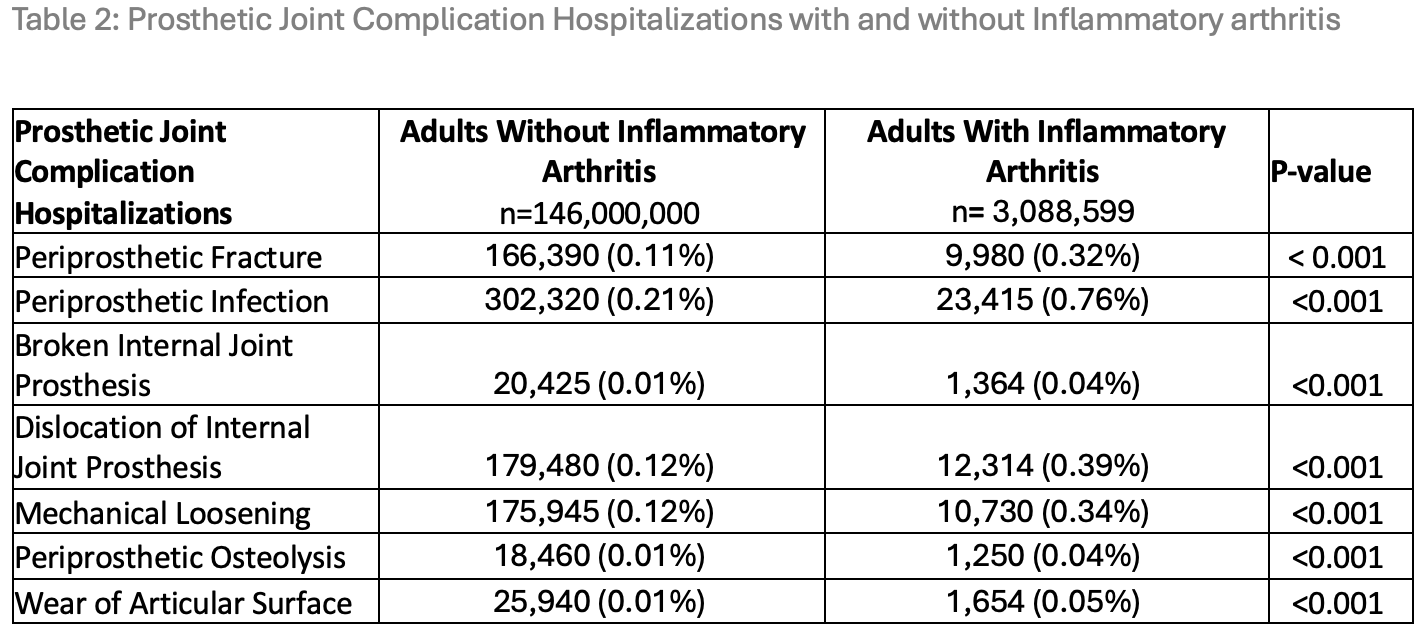
Results: We identified a total of 869,519 PJC hospitalizations out of which 54,705 (6.3%) had a concomitant diagnosis of IA. There were several epidemiological differences between the two groups of PJC hospitalizations those with and without IA (Table 1). Those with IA were younger (median, IQR age 68, 61-75 vs 69, 61-78, P value < 0.001), had higher proportion of females (75% vs 57%, P value < 0.001), had a marginally higher proportion of minorities (African-Americans, 9% vs 8%, P value 0.015 , Hispanics, 6% vs 5%, P value < 0.001 and Native Americans, 0.8% vs 0.5%, P value < 0.001) and were more likely to have Medicare insurance (72% vs 68%, P value < 0.001) and less likely to be privately insured (20% vs 21%, P value < 0.001) in comparison to those without IA. Sepsis was more common in the IA group (7% vs 6%, P value < 0.001) with longer length of stay (median, IQR 4, 2-7 vs 4, 2-6, P value < 0.001) and higher total hospital charges (Table 1). Overall unadjusted mortality was lower in the IA group (0.7% vs 1%, P value 0.11) in comparison to the non-IA group. All individual PJC (periprosthetic fracture, infection, osteolysis, broken internal joint prosthesis, dislocation, mechanical loosening, and wear of articular surface) were higher in those with IA than those without concomitant IA (P value < 0.001) (Table 2).
Conclusion: Out of all PJC hospitalizations, 1 in 16 had a concomitant diagnosis of chronic inflammatory arthritis. Those with IA were younger, more often female, and exhibit higher comorbidity burden, which translated to slightly longer hospital stay and higher total charges. IA patients were more susceptible to sepsis as well as all individual prosthetic joint complications in comparison to those without IA.
To cite this abstract in AMA style:
Sengupta A, Sami F, Arora S. Nationwide Analysis of Prosthetic Joint Complications with and Without Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/nationwide-analysis-of-prosthetic-joint-complications-with-and-without-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nationwide-analysis-of-prosthetic-joint-complications-with-and-without-inflammatory-arthritis/