Session Information
Date: Tuesday, November 14, 2023
Title: (1913–1944) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Sarcoidosis is multisystem autoimmune disease characterized by noncaseating granulomas which can result in significant morbidity and mortality. This study aims to identify variables associated with in-hospital death for sarcoid patients on a national level.
Methods: We performed a retrospective study of adult sarcoid hospitalizations from 2016-2020 National Inpatient Sample (NIS) database. Diagnoses for each hospitalization were identified by ICD-10 codes. We sought to identify predictors of in-hospital death among sarcoid patients. Variables were selected from literature review and ranking of common diagnoses among sarcoid inpatients. Variables with a p value ≤ 0.2 in the univariable screen were included in a multivariable logistic regression model. P values ≤ 0.05 were considered significant in the multivariable analysis.
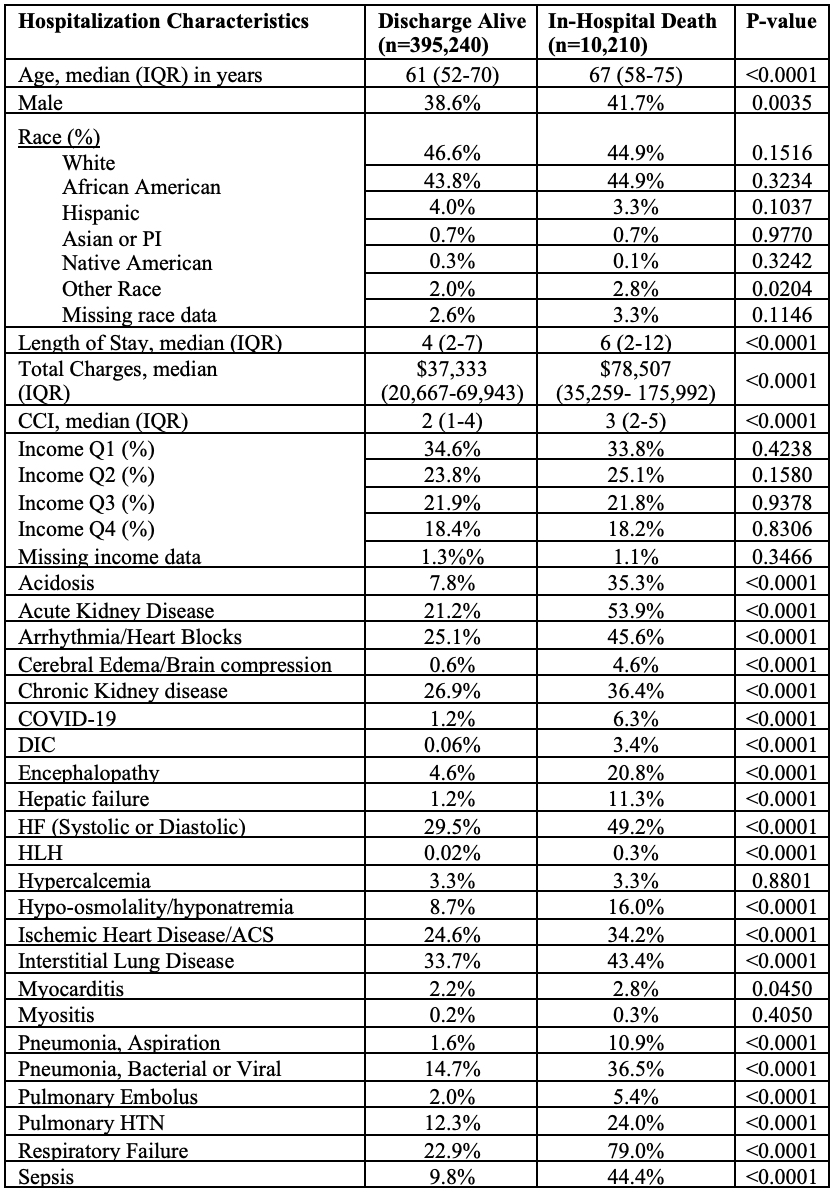
Results: There were 405,450 inpatient admissions with a diagnosis of sarcoidosis in the 2016-2020 NIS database. Of those, 10,210 (2.5%) died while in the hospital (table 1). The deceased group was older (median age 67 vs 61 years; p< 0.0001), had more males (41.7% vs 38.6%; p=0.0035), had longer median LOS (6 vs 4 days; p< 0.0001), had higher median total hospital charges ($78,507vs $37,333; p< 0.0001), and higher Charlson comorbidity index (CCI) (3 vs 2; p< 0.0001). Univariable analysis showed many variables associated with in-hospital death among sarcoid patients (table 2). Multivariable analysis showed the following variables were independently associated with a higher odds of in-hospital death: Age (OR 1.03; 95% CI 1.023 -1.032), CCI (OR 1.14; 95% CI 1.102-1.170), COVID-19 (OR 2.69; 95% CI 2.133-3.384), male gender (OR 1.16; 95% CI 1.047-1.290), other race (OR 1.79; 95% CI 1.275-2.505), acidosis (OR 2.46; 95% CI 2.190-2.755), Acute kidney failure (AKF) (OR 1.89; 95% CI 1.695-2.107), arrhythmia/heart blocks (OR 1.58; 95% CI 1.414-1.767), cerebral edema/brain compression (OR 8.29; 95% CI 6.177-11.115), disseminated intravascular coagulation (DIC) (OR 11.87; 95% CI 6.417-21.948), encephalopathy (OR 1.81; 95% CI 1.574-2.082), hepatic failure (OR 4.28; 95% CI 3.446-5.319), hemophagocytic lymphohistiocytosis (OR 5.43; 95% CI 1.269-23.212), aspiration pneumonia (OR 1.89; 95% CI 1.557-2.300), pulmonary embolus (OR 2.18; 95% CI 1.697-2.793), pulmonary hypertension (OR 1.22; 95% CI 1.079-1.383), respiratory failure (OR 6.70; 95% CI 5.911-7.592), and sepsis (OR 2.81; 95% CI 2.494-3.156) (table 3).
Conclusion: Our analysis showed that 2.5% of inpatient admissions carrying a sarcoid diagnosis ended in death. Demographic factors such as age, gender, other race, and CCI were independently associated with higher odds of mortality, while African American race and income quartile were not. Several comorbidities were independently associated with higher odds of in-hospital death: acidosis, acute kidney failure, arrhythmia/heart blocks, cerebral edema/brain compression, DIC, encephalopathy, hepatic failure, HLH, aspiration pneumonia, PE, pulmonary hypertension, respiratory failure, and sepsis. Clinicians should remain vigilant for these life-threatening complications since early recognition and intervention may improve inpatient sarcoid outcomes.
Abbreviations: ACS=Acute Coronary Syndrome; CCI= Charlson Comorbidity Index; CKD=Chronic Kidney Disease; DIC=Disseminated Intravascular Coagulation; IQR=Interquartile Range; HF=Heart Failure; HLH= Hemophagocytic lymphohistiocytosis; HTN=Hypertension; n= number; PI=Pacific Islander; Q=Quartile
Abbreviations: ACS=Acute Coronary Syndrome; CCI= Charlson Comorbidity Index; DIC=Disseminated Intravascular Coagulation; HF=Heart Failure; HLH= Hemophagocytic Lymphohistiocytosis; HTN=Hypertension; NIS=National Inpatient Sample Database; PI=Pacific Islander; Q=Quartil
Abbreviations: ACS=Acute Coronary Syndrome; CCI= Charlson Comorbidity Index; DIC=Disseminated Intravascular Coagulation; HF=Heart Failure; HLH= Hemophagocytic Lymphohistiocytosis; HTN=Hypertension; NIS=National Inpatient Sample Database
To cite this abstract in AMA style:
Manansala M, Sami F, Arora S, Manadan A. Nationwide Analysis of Predictors of Sarcoid Inpatient Mortality [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/nationwide-analysis-of-predictors-of-sarcoid-inpatient-mortality/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nationwide-analysis-of-predictors-of-sarcoid-inpatient-mortality/