Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Rheumatic diseases have a higher risk of cardiovascular events, particularly those related to atherothrombosis which represents the leading cause of premature mortality in most of these conditions. The increased risk may be explained by the presence of accelerated atherosclerosis, chronic inflammation, glucocorticoid use and autoimmune antibodies. Spontaneous coronary artery dissection (SCAD) is an infrequent cause of myocardial ischemia with an incidence of less than 1%. Recent evidence suggests that SCAD pathogenesis is non-inflammatory and there is no association between SCAD and rheumatologic conditions.
Methods: We conducted a retrospective review of 2016-2020 National Inpatient Sample (NIS) database. All acute coronary syndrome (ACS) adult hospitalizations were selected as our study population and were subdivided into SCAD (ICD-10 code I25.42) with and without rheumatologic conditions. Rheumatologic conditions included were: Ankylosing Spondylitis, Antiphospholipid Syndrome, Dermatomyositis/Polymyositis, Polymyalgia Rheumatica, Psoriasis or Psoriatic Arthritis, Rheumatoid Arthritis, Systemic Sclerosis limited or diffuse, Sjogren’s Syndrome, Systemic Lupus Erythematosus, Takayasu’s arteritis and vasculitis either Granulomatosis with Polyangiitis (GPA), Eosinophilic GPA or Polyarteritis Nodosa. Outcomes were adjusted for hypertension and hyperlipidemia as this have significant impact in SCAD mortality.
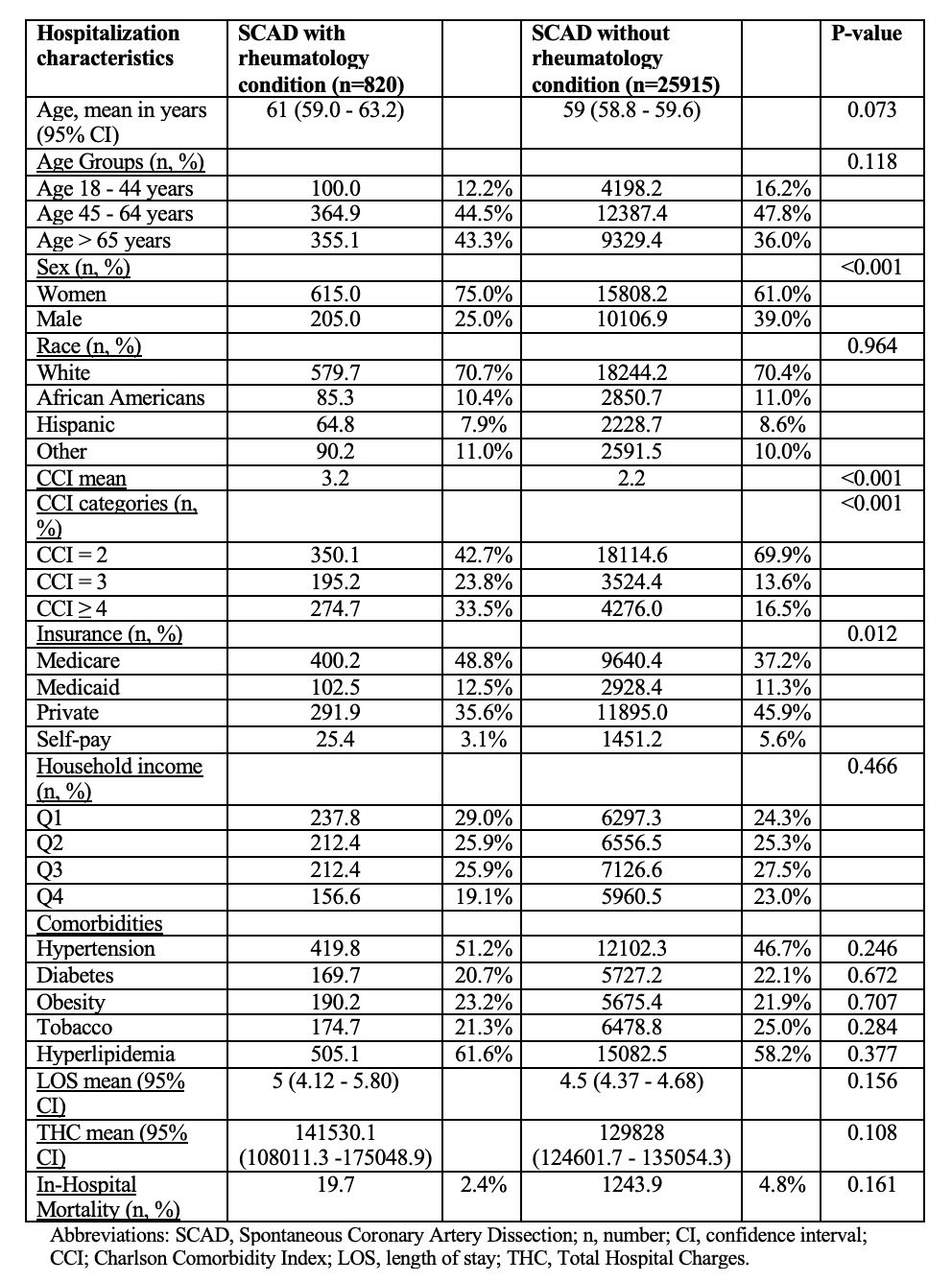
Results: There were 3,136,259 adult hospitalizations with ACS in the 2016 to 2020 NIS database. Of those, 820 had SCAD associated with rheumatologic condition. Compared to hospitalizations with SCAD and non-rheumatologic conditions (Table 1), the rheumatologic group was older (median age 61 vs 59 years; p=0.073), had more females (75% vs 61%; p< 0.001), similar proportion of Whites (70.7% vs 70.4%; p=0.964), less African Americans (10.4% vs 11%; p=0.964), less Hispanics (7.9% vs 8.6%; p=0.964), higher CCI mean (3.2 vs 2.2; p< 0.001), higher length of stay (LOS) (5 vs 4.5; p=0.156), higher median total hospital charges ($141,530.1 vs $129,828; p=0.108) and lower in-hospital mortality (2.4% vs 4.8%; p=0.161). Insurance and house-hold income was similar between the 2 groups. In terms of comorbidities, the rheumatologic group had more hypertension (51.2% vs 46.7%; p=0.246), lower diabetes (20.7% vs 22.1%; p=0.672), more obesity (23.2% vs 21.9%; p=0.707), less tobacco use (21.3% vs 25%; p=0.284) and more hyperlipidemia (61.6% vs 58.2%; p=0.377). Multivariable analysis showed that rheumatologic conditions were associated with lower odds of SCAD (OR 0.72; p < 0.001, 95% C.I. 0.607 – 0.864). Also, rheumatologic conditions had lower odds of mortality in patients with SCAD (OR 0.41; p=0.082, 95% C.I. 0.152 – 1.121).
Conclusion: Despite having a higher burden of comorbidities, patients with rheumatologic conditions had lower odds of both SCAD and mortality, though the latter finding was not statistically significant. Patient with SCAD were less likely to have any rheumatologic comorbidities than other patients admitted for ACS but without SCAD.
To cite this abstract in AMA style:
Romero Noboa M, El Sharu H, Cornejo D, Litvin R, Razok A. Nationwide Analysis of Adult Hospitalizations with Rheumatologic Conditions and Spontaneous Coronary Artery Dissection [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/nationwide-analysis-of-adult-hospitalizations-with-rheumatologic-conditions-and-spontaneous-coronary-artery-dissection/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nationwide-analysis-of-adult-hospitalizations-with-rheumatologic-conditions-and-spontaneous-coronary-artery-dissection/