Session Information
Date: Tuesday, November 9, 2021
Title: Pediatric Rheumatology – Clinical Poster III: Miscellaneous Rheumatic Disease (1614–1644)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Nailfold capillary microscopy (NCM) is a cornerstone in the diagnosis of Systemic Sclerosis (SSc) in adulthood. Although Raynaud’s phenomenon (RP) is common in childhood, studies on diagnostic methods to differentiate between primary RP (PRP) and secondary RP (SRP) at a young age are scarce. The aim of this study was to determine the value of NCM in differentiating between PRP and SRP in children and adolescents with RP.
Methods: In this nested case-control study, 83 patients diagnosed with RP and having undergone NCM in childhood were retrospectively included. Based on whether they were diagnosed with a connective tissue disease (CTD) during follow-up, patients were classified as PRP or SRP. Patients were considered to have SRP if they had received a CTD diagnosis based on current ACR/ EULAR classification criteria: SSc, Mixed CTD (MCTD) systemic lupus erythematosus (SLE), adult and juvenile idiopathic inflammatory myopathies (IIM), rheumatoid arthritis (RA) primary Sjögren’s syndrome (SS). NCM was judged visually by a vascular technician. PRP and SRP patients were compared on demographics, NCM, and serology. Variables associated with SRP were included in a multivariate logistic regression model. Predictive values were calculated for NCM, ANA positivity, and the combination of NCM and ANA positivity.
Results: At the time of the NCM, the mean age of the RP patients was 15.4±2.3 years (Table 1). Of these patients, 78% were classified as PRP and 22% as SRP at mean follow-up of 6.4±3.20 years. Of the SRP patients, 22% had an undifferentiated CTD, 22% had a MCTD, 17% had SLE, 11% had IIM, 6% had SSc, 6% had SS, 6% had incomplete SLE, 6% had incomplete SSc and 6% had incomplete SS. In total, half of patients had dilated capillaries, 25% had giant capillaries, 22% had capillary los, 17% had hemorrhages. Giant capillaries were confined to patients with SSc (1 out of 1), MCTD (3 out of 4), and IIM (2 out of 2). An SSc-like NCM pattern was observed in only 25%, which did not differentiate between those who developed CTD and those who did not. Of the NCM parameters, only capillary loss was associated with SRP (p=0.01). In a multivariate logistic regression model, capillary loss was an independent predictor (OR=3.98, CI 95% 1.22-12.99) (Table 2). After including ANA in the model, capillary loss was not an independent predictor of SRP. Capillary loss had a sensitivity of 44% and a specificity of 84% for SRP. PRP was correctly predicted in 99%, while SRP was correctly predicted in 27% of the cases by using capillary loss. ANA combined with capillary loss had a sensitivity of 67% and a specificity of 86% (Table 3).
Conclusion: Of all NCM findings, only capillary loss was predictive of SRP in children presenting with RP. Using NCM in childhood should be done with caution since the majority of children developing future CTDs present without specific NCM abnormalities. However, if present, capillary loss on NCM has a high specificity for future CTD. Because of this, we believe NCM could be useful as a screening method to exclude SRP when combined with serology. Our study underlines that future research should determine the predictive value of NCM and its specific abnormalities for individual CTDs in children presenting with RP.
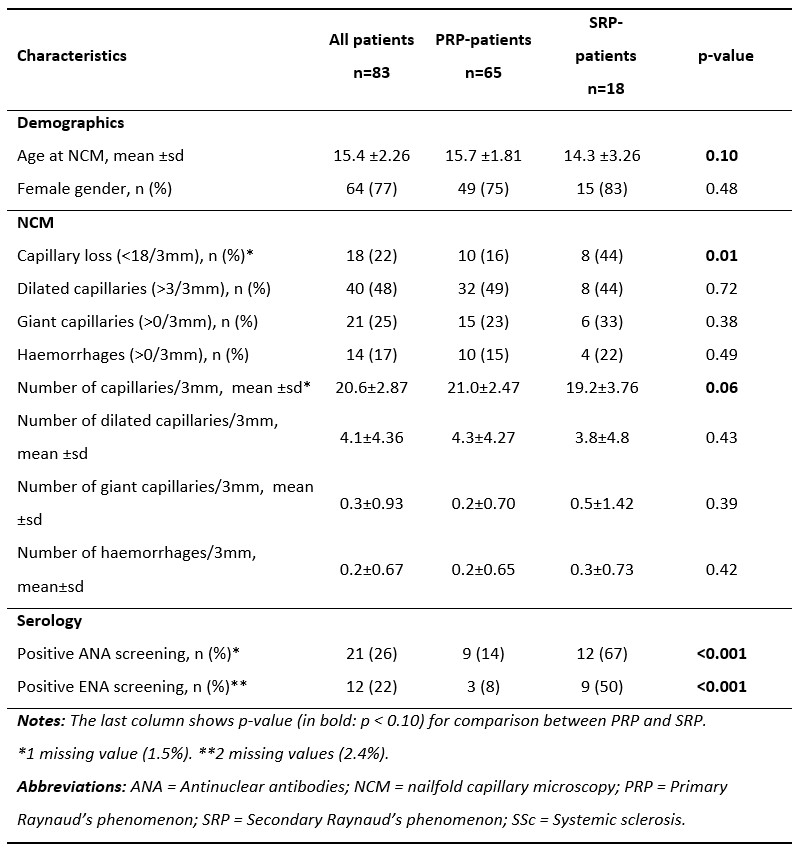 Table 1: Baseline characteristics for the whole study population, and the PRP group and SRP group separately.
Table 1: Baseline characteristics for the whole study population, and the PRP group and SRP group separately.
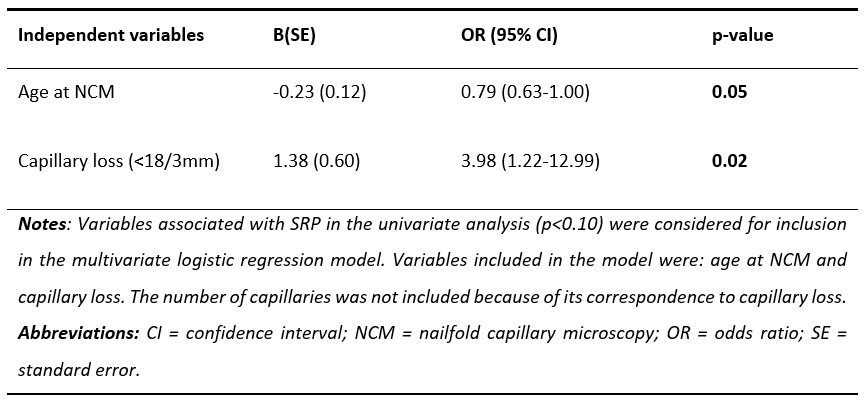 Table 2: Multivariate logistic regression model showing predictive value of baseline variables for SRP excluding ANA positivity.
Table 2: Multivariate logistic regression model showing predictive value of baseline variables for SRP excluding ANA positivity.
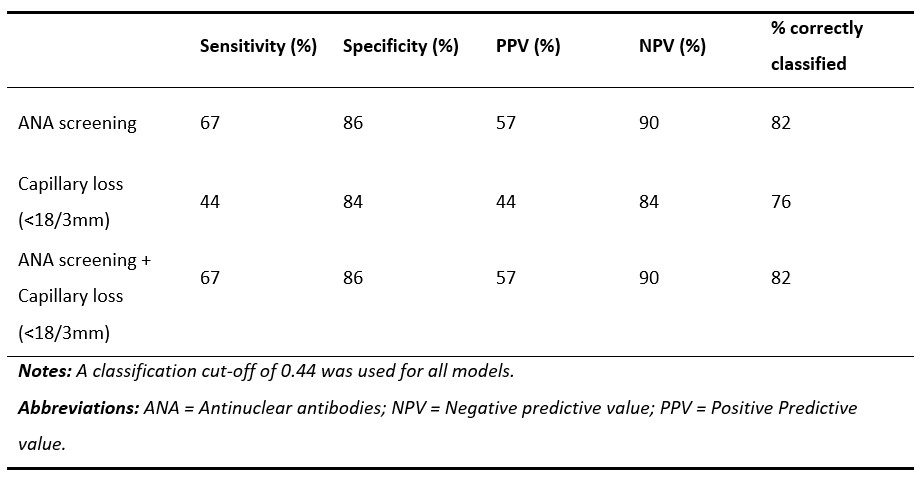 Table 3: Predictive value of logistic regression models comprising different independent variables for prediction of SRP.
Table 3: Predictive value of logistic regression models comprising different independent variables for prediction of SRP.
To cite this abstract in AMA style:
Farenhorst C, Van Roon A, van Gessel A, Stel A, Bootsma H, Armbrust W, Mulder D. Nailfold Capillary Microscopy in Children with Raynaud’s Phenomenon. Potential Predictive Value of Capillary Loss for Future Connective Tissue Disease? [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/nailfold-capillary-microscopy-in-children-with-raynauds-phenomenon-potential-predictive-value-of-capillary-loss-for-future-connective-tissue-disease/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nailfold-capillary-microscopy-in-children-with-raynauds-phenomenon-potential-predictive-value-of-capillary-loss-for-future-connective-tissue-disease/
