Session Information
Date: Monday, November 13, 2023
Title: (1124–1154) Miscellaneous Rheumatic & Inflammatory Diseases Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Idiopathic inflammatory myopathies (IIM) are a heterogeneous group of acquired muscle diseases, which have distinct clinical, pathological and histological features. Autoantibodies are clinically useful biomarkers to help the diagnosis of IIM. Raynaud’s phenomenon is very frequent and the presence of microvascular changes in IIM have been described however, the role of nailfold videocapillaroscopy NVC) for diagnosis and prognosis in IIM is not clearly established. The aim of this study was to study the relationship between clinical and immunological characteristics and nailfold videocapillaroscopy (NVC) abnormalities in patients with idiopathic inflammatory myopathies (IIMs).
Methods: We performed a retrospective study of IIM patients followed in a University Hospital. Patients underwent a NVC at 200x magnification. Epidemiological, clinical data and antibody status, including myositis and scleroderma antibody panel of all patients was retrieved. NVC findings including loss of capillary density, enlarged and giant capillaries, ramified capillaries, haemorrhages, thrombosis, avascular areas, disorganization of capillary architecture and subpapillary venous plexus presence were recollected, if present. For the comparison of qualitative and/or quantitative variables Fisher’s exact Test or T-test was performed when necessary.
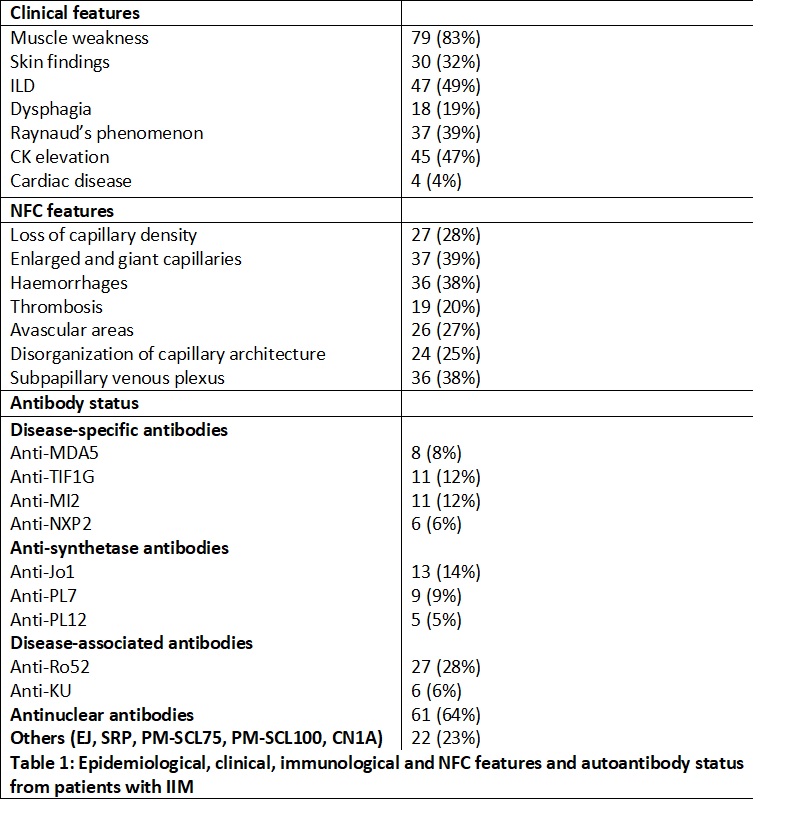
Results: 95 patients with NVC performed during the follow-up were included (66% female) with a median age at inclusion of 55.3±24 years. Median IIM duration was 6.8±7 years. 39% had Raynaud’s phenomenon at first clinical evaluation and 58% of them showed NVC pathological findings. Table 1 Summarizes the epidemiological, clinical, and autoantibody status of the patients. We found an association between the presence of dysphagia and avascular areas (p=0.02) or abnormal capillary organization (p< 0.01) on NVC. ILD was associated with capillary loss (p=0.04) and avascular areas (p=0.004). Anti-MDA5+ was associated with capillary loss (p=0.03), thrombosis (p=0.02) and ramified capillaries (p=0.04). Anti-Mi2+ and anti-Th/To was associated with abnormal capillary organization (p=0.017 and p=0.001). The presence of haemorrhages was associated with anti-Ku+ (p=0.048) and anti-PL12+ (p=0.046). The presence of enlarged capillaries was associated with anti-RNA-pol III (p=0.04) and anti-NXP2 (p=0.044). A significant association between anti-Ro52 (OR 2.69, CI 95% 1.05-6.8, p 0.03) and anti-Jo1 (OR 7.03 CI 95% 1.46-33.7, p 0.01) with ILD was found. Anti-PML (OR 4.32 CI 95% 1.35-10.42, p 0.038) and anti-Th/To (OR 5.82 CI 95% 1.89-13.24, p 0.04) were associated with dysphagia. Anti-MDA5 (OR 5.85 CI 95% 1.92-14.21, p 0.044) was associated with skin involvement.
Conclusion: The presence of certain autoantibodies is related to the degree of microangiopathy in IIM and associates with capillaroscopic changes. Studying the association between capillaroscopic changes with diagnostic and pathogenic autoantibodies in IIM can provide useful information regarding the current knowledge about pathogenesis, classification, and prognosis of the disease.
To cite this abstract in AMA style:
Sieiro Santos C, Tandaipan J, Mariscal A, Sainz-Comas L, Codes H, Moya P, Magallares-Lopez B, Martínez Martínez L, Millán Arciniegas A, Sang Park H, Díaz-Torné C, Laíz Alonso A, Fernández S, Ros S, Corominas H, Díez Álvarez E, Castellvi I. Nailfold Capillaroscopy Findings in Patients with Idiopathic Inflammatory Myopathies and Its Association to Autoantibodies [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/nailfold-capillaroscopy-findings-in-patients-with-idiopathic-inflammatory-myopathies-and-its-association-to-autoantibodies/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nailfold-capillaroscopy-findings-in-patients-with-idiopathic-inflammatory-myopathies-and-its-association-to-autoantibodies/